Does Your Baby Have a Tongue or Lip Tie?
Painful, cracked, compressed-after-breastfeeding nipples. Baby not gaining weight well. Constant breastfeeding sessions that seem to take over an hour. Excessive baby fussiness and gas. These are some of the many signs that your child may have a tongue and/or lip tie. So, what is a tongue and lip tie and how do they affect breastfeeding? What are ways to fix them and improve breastfeeding?
With several fantastic articles already written on this subject, we are going to give brief answers to these questions and link to our favorite comprehensive resources. Also, over the next month, we will be sharing stories from breastfeeding mothers whose babies had tongue and/or lip ties.
Painful, cracked, compressed-after-breastfeeding nipples. Baby not gaining weight well. Constant breastfeeding sessions that seem to take over an hour. Excessive baby fussiness and gas. These are some of the many signs that your child may have a tongue and/or lip tie. So, what is a tongue and lip tie and how do they affect breastfeeding? What are ways to fix them and improve breastfeeding?
With several fantastic articles already written on this subject, we are going to give brief answers to these questions and link to our favorite comprehensive resources. Also, over the next month, we will be sharing stories from breastfeeding mothers whose babies had tongue and/or lip ties.
What is a tongue tie and lip tie?
There are pieces of connective membranes under the tongue and behind the upper lip called frenula. Everyone has a lingual (tongue) frenulum and a labial (lip) frenulum, which means that if your baby has one, it doesn’t automatically mean that you are going to have breastfeeding challenges. It’s how the tongue and upper lip function that determine if the frenula are causing a problem.
Tongue tie
Upper lip tie
How do tongue and lip ties cause breastfeeding challenges?
When the frenula are tight, they act like rubber bands, tethering down the tongue to the base of the mouth or the upper lip close to the upper gumline. This makes it difficult to move the tongue in an effective manner or flange the upper lip out. When the tongue doesn’t have full range of motion, it can cause all sorts of issues. Some moms’ nipples will be compressed, causing pain and ineffective milk extraction. Some babies will become very tired and fatigued while breastfeeding, having to work extra hard to compensate for the lack of range of motion in their tongues. This can turn into ineffective, long feedings and slow weight gain for babies. Other babies gain weight perfectly fine, but have tons of gas and excessive fussy periods because they are taking in so much air while breastfeeding due to the inability to push the milk back in a wavelike motion. Babies with tongue ties or significant lip ties often continually fall off the breast, as they are unable to form a good seal and suction. Other babies have such difficulty latching on to the breast that they refuse to breastfeed altogether.
Here are two articles that describe how tongue and lip ties can affect breastfeeding:
A Breastfeeding Mom’s Symptoms are as Important as Baby’s
Baby’s Weight Gain is Not the Only Marker of Successful Breastfeeding
Why didn’t my healthcare provider mention this to me?
Most health care providers have not been trained to assess and diagnose tongue or lip ties. Again, it is how the tongue and lip function (or not function) that cause the breastfeeding challenges. Most health care providers have not been trained to complete suck assessments on infants, therefore they cannot accurately assess what the tongue is doing while feeding. The best person to assess for a tongue or lip tie is a trained IBCLC (International Board Certified Lactation Consultant).
Who can treat my child’s tongue and/or lip tie and what are my options?
The best person to diagnose and treat a tongue or lip tie is a trained dentist, ENT (Ear, Nose, and Throat surgeon), oral surgeon, naturopath, pediatrician, or other medical professional trained to do minor surgery. Make sure to do your research, as not all professionals that revise tongue and lip ties know how to release them effectively. If the professional doesn’t do the revision procedure effectively and completely, then it will not fix the breastfeeding challenges completely and your baby may have to have the procedure again.
In most cases, the tongue or lip tie revision is done at an office visit. Some practitioners will numb the area before the procedure, although it isn’t necessary. Some practitioners, such as ENTs and pediatricians, may use blunt-edged scissors to snip the tight frenulum. Others, such as dentists, may use laser for the revision procedure.
Are there any negatives to having the tongue or lip tie revised?
There is very little risk for having your baby’s tongue or lip tie revised. Most parents comment after the procedure that their only regret is that they didn’t do it sooner, as it improved their breastfeeding challenges tremendously. Some babies may be a little fussy after the procedure, but most will settle with some extra cuddles. Some parents find that a little infant tylenol or homeopathy can help relieve pain (but always check with your healthcare provider for appropriate dosing.)
How can I keep the frenulum from scarring down after the procedure?
It is very important that parents do suck and stretching exercises after the procedure to prevent scarring down. My colleague, Melissa Cole, IBCLC, created this quick and easy video for suck exercises after tongue tie revisions: http://vimeo.com/55658345. She recommends doing these a few times a day, during baby’s quiet alert time, to retrain baby’s tongue to suck effectively and to prevent scarring down. A local dentist recommends bending baby’s upper lip up to his/her nose after an upper lip tie release to prevent scarring down.
Will my breastfeeding challenges resolve immediately after the procedure?
Most moms report some immediate improvement after the procedure, but it can sometimes take up to a few weeks or months to resolve all of your breastfeeding challenges, depending on other confounding issues, such as mom’s milk supply or baby’s progress. Remember, your baby has been using his/her tongue and upper lip in this way since he/she was in utero, so it may take some time to ‘relearn’ how to use his/her tongue and upper lip effectively. Body work, such as craniosacral therapy and chiropractic, can help speed up this process as it can reset your baby’s nervous system, as well as relax the muscle tension that your baby may have developed while using compensating mechanisms.
Here are some additional online resources that have excellent information about tongue and lip ties. Stay tuned for our featured stories from moms whose breastfeeding challenges improved after having their babies’ tongue and lip ties revised. Better yet, sign up for our newsletter and have these articles delivered directly to your email inbox!
Websites that offer ways to see if your baby might be tongue tied:
Catherine Watson Genna: Is My Baby Tongue Tied?
Dr. James Ochi: Tongue Tie Survey
More researched-based articles about tongue and lip ties:
American Academy of Pediatrics Tongue Tie article
Dr. Kotlow: Tongue Tie Fact Sheet
The Leaky Boob: The Basics of Tongue and Lip Tie: Related Issues, Assessment, and Treatment
Boob Group episode: Tougue Ties and Lip Ties: Symptoms, Treatment, and Aftercare
If you would like to submit your personal story about breastfeeding a baby with a tongue or lip tie, please email it to robinkaplan@sdbfc.com
Did your baby have a tongue or lip tie?
How did this affect breastfeeding?
What Every Mom Should Know About Breastfeeding During the Early Weeks
How much breast milk does my baby need per feeding?
What is common nursing behavior for a newborn?
How will I know that my baby is getting enough?
As a new mom, these are common questions that you may ask your pediatrician, midwife, postpartum nurse, family, and friends and GUESS WHAT..... they may all have a different answer!
How much breast milk does my baby need per feeding?
What is common nursing behavior for a newborn?
How will I know that my baby is getting enough?
As a new mom, these are common questions that you may ask your pediatrician, midwife, postpartum nurse, family, and friends and GUESS WHAT..... they may all have a different answer!
How complicated is that?
Sometimes you may feel like there are ‘too many cooks in the kitchen’ and that all of the advice you receive contradicts what you just heard from someone else 5 minutes ago.
Talk about frustrating!
Well, one of our goals at the San Diego Breastfeeding Center is to make breastfeeding as seamless and uncomplicated as possible. We want to empower moms with knowledge and confidence to get breastfeeding off to a great start!
After listening to local moms express discontent about hearing contradictory breastfeeding information, we decided to do something about it. First, we canvased our local breastfeeding mamas and asked, “What information do you wish you would have known about breastfeeding during those early weeks?” Then we hired one of those awesome mamas, Elisa Suter, of Paper Doll Design Studios, to design a brochure that shares our top tips that every mom (and pediatrician) should know about breastfeeding during the early weeks.
Here is the final product! Isn’t it beautiful? We hope that this brochure provides the clear, consistent, evidence-based breastfeeding information our mamas are looking for.
If you live in San Diego and would like us to deliver these brochures to your pediatrician's office, please email us at robinkaplan@sdbfc.com.
If you live outside of San Diego and would like to order the Adobe file to personalize this brochure for YOUR local pediatricians and clients, please email us at robinkaplan@sdbfc.com
Breastfeeding Misconceptions: Does Baby Weight Loss Mean Mom Doesn’t Have Enough Milk?
How many times have you heard a so-called ‘fact’ from a family member, friend, healthcare professional, or online resource that has your ‘mama-radar’ going off at warp speed? Maybe something just doesn’t sound right. Maybe it goes against all of your mama-bear instincts. Maybe it is completely contradictory to what you heard the previous day. Well, it’s time to start busting those myths and misconceptions!
Today, we start our new series called Breastfeeding Misconceptions.
Every month we will be BUSTING common breastfeeding myths and misconceptions, hopefully making your breastfeeding experience that much easier!
How many times have you heard a so-called ‘fact’ from a family member, friend, healthcare professional, or online resource that has your ‘mama-radar’ going off at warp speed? Maybe something just doesn’t sound right. Maybe it goes against all of your mama-bear instincts. Maybe it is completely contradictory to what you heard the previous day. Well, it’s time to start busting those myths and misconceptions!
Today, we start our new series called Breastfeeding Misconceptions.
Every month we will be BUSTING common breastfeeding myths and misconceptions, hopefully making your breastfeeding experience that much easier!
Myth #1: If your baby loses weight in the first week, it means your milk supply is low.
Not true!
All babies lose weight after birth:
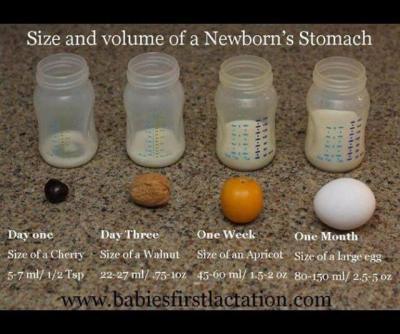
A newborn baby takes in approximately 5-7ml of colostrum per feeding in the first 24 hours. Babies are burning more calories than that as they attempt to breastfeed and expel that sticky, gooey meconium. Nature has provided the perfect amount of colostrum in those first few days to nourish your baby and while the quantity is small, the quality is jam-packed with every calorie, immunological property, protein, vitamin, and laxative that your newborn needs to poop and pee. Babies are expected to lose weight in those first few days. That doesn’t mean that mom’s supply is low.
Babies typically lose weight until mom’s ‘fuller milk’ comes in:
The amount of colostrum continues to grow as your milk transitions to ‘fuller milk’, which comes in around 2-5 days (depending on baby’s access to breast, effective sucking, birth interventions, etc.) Typical colostrum amounts are about 5-7 ml per feeding in first 24 hours, 7-15ml per feeding from 24-48 hours, and 22-27ml per feeding from 48-72 hours. Your baby will most likely lose weight until your ‘fuller milk’ comes in, but that doesn’t necessarily mean that you don’t have enough milk. What parents want to look for is that their baby is peeing and pooping (at least 1 of each per day of life) and baby’s weight loss plateaus once mom’s fuller milk has come in.
Here’s a great graphic of a baby’s stomach from Babies First Lactation and Education
Delayed milk supply doesn’t equal low milk supply:
There are several situations where a mother is at a higher risk for a delayed milk supply. As mentioned in this Best for Babes article, there are a number of factors that increase a mother’s risk for delayed milk supply. Some are beyond our control (or difficult to control): diabetes, obesity, thyroid problems, hypertension, PCOS, preterm birth, and anemia. There are also factors related to birth that can influence when a mother’s fuller supply comes in: cesarean birth, receiving lots of IV fluids, prolonged pushing stage, stress, cascade of interventions, hemorrhaging, mother-baby separation, just to name a few. If you are at a higher risk for having a delayed milk supply, it can be very helpful to speak with a lactation consultant within the first 24 hours after your baby is born. She can teach you ways to hand express and pump to help speed up the process of your fuller milk coming in, thereby DECREASING your risk for a low milk supply.
Lots of fluid during labor can cause greater weight loss in babies:
Studies have shown that mothers who have long periods of birth interventions (epidural, Pitocin, eventual emergency cesarean, etc.), tend to have more fluids during labor, thereby inflating baby’s birth weight and causing a large drop in baby’s weight in the first 24 hours. In those first 24 hours, we are looking for 1 pee and 1 stool (as a minimum.) For those babies that pee and stool multiple times in the first 24 hours, their weight loss is going to be greater, but that is not an indicator that mom’s supply is low. It just means they had a lot of fluids to expel after birth. Here are a few articles that explain this phenomenon. Dr. Jen: Newborn Weight and The Boob Group: Birth Interventions and Their Impact on Breastfeeding.
Baby may lose weight (or gain weight really slowly) because they are having a difficult time transferring mom’s milk:
There are many reasons why a baby might lose weight, sometimes continuing past the first week of life, even when mom has a full supply. Some of these include: engorgement (causing baby to have difficulties latching on), tongue-tie or lip tie, baby is recuperating after a difficult labor, baby is jaundiced, premature baby, etc. Again, when baby is losing weight due to these situations, it doesn’t always mean that mom’s supply is low. If her baby is having a difficult time transferring milk, then she should definitely meet with a lactation consultant to make sure she is doing everything she can to protect her milk supply until her baby can start to efficiently transfer milk from her breast.
Supplementation doesn’t equal formula:
If your milk supply is delayed, if your baby has elevated bilirubin, if your baby has lost more than 10% of his/her birth weight, that doesn’t automatically equal FORMULA supplementation. Mom may actually have enough of her own milk to supplement her baby with until baby’s weight is back on track. All she has to do is hand express or pump and see what extra she has. If mom doesn’t have enough of her own milk to supplement, then the hand expression or pumping (in addition to breastfeeding) will help to bring in her milk supply more fully. In the meantime, moms have other options. A mom can use milk bank breast milk or donor milk, if she prefers. For terrific information about milk banks, check out Human Milk Banking Association of North America and for milk sharing, check out Eats on Feets. The most important take away of this all…. When supplementation is necessary, it is imperative for a mom to increase her breast stimulation to help bring in her supply more fully. When her baby is getting a supplementation from another source, it is saying to mom’s body that she doesn’t have to make that amount of milk, which is totally not the case. The sooner mom’s fuller milk comes in, the sooner supplementation can decrease, so spend the extra time and effort… it will be worth it in the end.
Important note: When you might become concerned about your milk supply
While all of the above statements should illustrate why a mother should not be told that she has a low milk supply early on, there are some situations that might indicate that mom has a low milk supply (either temporarily or more long term.) If you are experiencing any of these situations, please connect with an IBCLC as soon as possible, as sometimes this can be a very temporary situation, as long as measures are taken quickly to protect mom’s milk supply. Here are some indicators that mom’s supply might be low:
Breasts did not grow and/or areola didn’t get darker during pregnancy
Breasts don’t feel heavier or fuller by 5-7 days postpartum
Fuller milk hasn’t ‘come in’ by 5-7 days postpartum
Baby is continuing to need supplementation to gain weight and mom is not making enough to supplement with her own milk
Mom has insufficient glandular tissue