Functional Nutrition for Pregnancy & Postpartum: Support Your Health and Your Baby’s Wellbeing
Pregnancy and postpartum are often painted as joyful seasons—but the truth is, they can also feel overwhelming, exhausting, and full of confusing symptoms. Maybe you’ve been told your bloating, constipation, or fatigue are “just part of postpartum.” Or that your baby’s fussiness is normal and they’ll eventually grow out of it. Perhaps you’ve even been advised to “just cut out dairy” without anyone looking deeper into what’s really going on.
Published Oct 5, 2025
Author: Robin Kaplan, M.Ed, IBCLC, FNC
Pregnancy and postpartum are often painted as joyful seasons—but the truth is, they can also feel overwhelming, exhausting, and full of confusing symptoms. Maybe you’ve been told your bloating, constipation, or fatigue are “just part of postpartum.” Or that your baby’s fussiness is normal and they’ll eventually grow out of it. Perhaps you’ve even been advised to “just cut out dairy” without anyone looking deeper into what’s really going on.
ABOUT SDBFC
The San Diego Breastfeeding Center was established in 2009 by Robin Kaplan, International Board Certified Lactation Consultant, Functional Nutritionist, and parent. Her vision was to create a judgment-free, inclusive support system for families navigating infant feeding challenges.
SDBFC offers a wide range of one-on-one breastfeeding, infant feeding, and nutrition consultations - as well as classes, support groups, online articles, and social media - making it your one-stop-shop for all things infant feeding!
Why Functional Nutrition Matters for Lactating Parents
Our medical history and diet play a huge role in shaping our gut microbiome. Over time, things like thyroid conditions, insulin sensitivity, PCOS, antibiotics, or food intolerances can cause inflammation in the body. This inflammation impacts how we digest food, absorb nutrients, process hormones like insulin and estrogen, and how our body feels overall.
When you’re producing milk, this becomes an even bigger part of the story. If your gut isn’t breaking down proteins well, your baby may react to some of the foods you eat—not because the food itself is “bad,” but because of how your body is processing it. That’s why simply removing dairy or waiting for your baby to “grow out of it” is often just a band-aid. Functional nutrition looks deeper at your health history to heal your gut, which in turn helps your baby digest your milk more comfortably.
And if antibiotics were given during pregnancy, labor, or postpartum, rebuilding “good” bacteria for both parent and baby can help remedy mucus in stool, colic-like symptoms, constipation, and yeast.
What if you didn’t have to just wait it out? With the right support, you can address the root causes of your symptoms, restore balance, and help both you and your baby thrive.
What is Functional Nutrition?
Functional nutrition connects the dots between symptoms and their root causes. Instead of quick fixes, it looks at diet, lifestyle, illness, stress, environment, and genetics to create a personalized plan that supports long-term health for you and your baby.
Who Benefits from a Prenatal Functional Nutrition Appointment?
Pregnancy is the perfect time to lay a strong foundation for both your health and your baby’s development. Functional nutrition may be especially helpful if you are:
Preparing for lactation after a history of low milk supply or breastfeeding/chestfeeding challenges
Managing conditions like PCOS, thyroid imbalance, or gestational diabetes
Looking for a holistic, evidence-based approach to support pregnancy and baby’s growth
Who Benefits from a Postpartum Functional Nutrition Appointment?
The postpartum period brings healing, shifting hormones, and new demands—especially if you’re lactating. Support may be most helpful for:
Adults with chronic inflammation, autoimmune conditions, PCOS, insulin resistance, or gut challenges
Lactating parents struggling with unexplained low supply, plugged ducts, or recurring breast infections
Parents or babies experiencing constipation, diarrhea, bloating, or other digestive discomfort
Babies with reflux, colic, suspected food intolerances, or yeast-related issues
Benefits of Meeting with a Functional Nutrition Counselor
One of the biggest benefits? Being heard. Instead of dismissing symptoms, functional nutrition helps uncover the why behind them—so you can heal and feel better long term. Outcomes may include:
Improved digestion and gut health (for parent and baby!)
Reduced inflammation and food/nutrient absorption
Enhanced immune function
Balanced hormones
Robust milk supply
Improved mood and mental health
Lower risk of chronic conditions like thyroid imbalance, insulin resistance, and autoimmune disorders
Do All Functional Nutrition Counselors Recommend Elimination Diets?
Not at all. Functional nutrition is personalized, not one-size-fits-all. While elimination diets can help identify food sensitivities, they’re not always needed.
Food journals may be used to spot patterns and triggers
If an elimination diet is suggested, it’s usually temporary. And we always provide replacement food recommendations and recipes!
The goal is to heal underlying issues so foods can be reintroduced
Recommendations may also include supplements and lifestyle changes for lasting results
Taking the Next Step
If you’re curious about whether functional nutrition could help during pregnancy or postpartum, the best place to start is with a conversation.
Here’s how to get started:
Book your appointment with our IBCLC + functional nutrition counselor, Robin Kaplan (SDBFC Founder and Owner!)
Fill out our comprehensive intake form so we can understand your full health picture, as well as your baby’s.
Begin your personalized journey with a plan designed just for you and your baby
Whether you’re navigating pregnancy, the early postpartum weeks, or beyond, functional nutrition can be the key to feeling more energized, balanced, and healthy. We can’t wait to help you and your baby thrive.
Don’t let milk supply or digestion troubles cause stress for you or your baby! At each functional nutrition appointment, our IBCLC/Functional Nutritionist completes a full medical history and lactation intake, discusses feeding patterns and symptoms, and offers strategies for supporting your milk supply and healing underlying conditions. Plus, if you are already working with a lactation consultant, we will work collaboratively to support their recommendations and weave in functional nutrition components! Book a one-on-one functional nutrition consultation today
SDBFC is committed to providing high-quality lactation and functional nutrition consultations to parents in San Diego and beyond. Explore our postpartum, prenatal, and functional nutrition consultations, take a breastfeeding class or attend a workshop.
About the Author
Robin Kaplan has been an IBCLC since 2009, the same year that she opened up the San Diego Breastfeeding Center. Robin was the founding host of the Boob Group podcast and published her first book, Latch: a Handbook for Breastfeeding with Confidence at Every Stage in 2018. Melding her passions for supporting lactating parents and holistic health, Robin finished her Functional Nutrition Certification in 2023. In her free time, she enjoys hanging out with her two teenage boys, hiking, traveling, weaving, cooking, and searching for the best chai latte.
Breastfeeding during Your Period: When Aunt Flow comes to visit
One of the many surprises of the postpartum journey is how your body responds to chest/breastfeeding—and that includes your period. Some parents enjoy months (or even years!) without a menstrual cycle, while others see their period return much sooner than expected. Let’s take a closer look at why your cycle may return (sooner rather than later), how it can impact chest/breastfeeding, and what you can do to support your body during this time.
Originally published on Oct 11, 2023; Revised Sept 30, 2025
Author: Robin Kaplan, M.Ed, IBCLC, FNC
One of the many surprises of the postpartum journey is how your body responds to chest/breastfeeding—and that includes your period. Some parents enjoy months (or even years!) without a menstrual cycle, while others see their period return much sooner than expected. Let’s take a closer look at why your cycle may return (sooner rather than later), how it can impact chest/breastfeeding, and what you can do to support your body during this time.
ABOUT SDBFC
The San Diego Breastfeeding Center was established in 2009 by Robin Kaplan, International Board Certified Lactation Consultant, Functional Nutritionist, and parent. Her vision was to create a judgment-free, inclusive support system for families navigating infant feeding challenges.
SDBFC offers a wide range of one-on-one breastfeeding, infant feeding, and nutrition consultations - as well as classes, support groups, online articles, and social media - making it your one-stop-shop for all things infant feeding!
When Will My Period Return While Breastfeeding?
Unfortunately, there’s no one-size-fits-all answer. Lactating does suppress your cycle for a while, but the timing is different for everyone. Some parents may not menstruate for months—or even years—while others see their period return within a few weeks or months.
Here are a few factors that can influence when your period returns:
How often your baby nurses
How often your baby receives a supplement (other than your milk) in a bottle
Whether your baby uses a pacifier
How long your baby is sleeping at night
If your baby has started solids
Your unique body chemistry and hormone balance
Typically, the more often your baby is at the chest/breast—day and night—the longer your period might be delayed. When you chest/breastfeed, your body produces high levels of prolactin. This hormone stimulates milk production but also suppresses the release of hormones necessary for ovulation and menstruation (like estrogen and progesterone).
Once your baby begins feeding less often—perhaps because of longer stretches of nighttime sleep or supplementation with something other than your milk—your prolactin levels drop, signaling your body to start ovulating again.
Will Breastfeeding Feel Different When My Period Returns?
For some parents, nothing changes at all. For others, hormonal shifts can bring a few noticeable differences, such as:
Nipple tenderness during ovulation and menstruation
A temporary dip in milk supply in the days leading up to your period
Baby wanting to nurse more often to compensate for lower milk volume
Baby feeding less, since some babies notice a slight change in the taste of milk
Baby getting frustrated at the chest/breast due to reduced flow
The good news? These changes are temporary. A few days into your period, your milk supply and nursing rhythm usually return to normal.
What Can I Do About a Temporary Dip in Milk Supply?
If you notice your supply dipping during your cycle, here are a few strategies to try:
Let your baby nurse as often as they want (it may feel like a short growth spurt).
Consider adding a daily magnesium glycinate supplement (120–240 mg at night) to support your body as hormone levels shift.
Increase iron-rich foods—like leafy greens, beans, and red meat—or consider a gentle supplement such as Floradix or Green Super Foods.
Add milk-boosting herbs (galactagogues) into your routine, if needed.
(Always consult your healthcare provider before starting any supplements or herbs.)
If you’re struggling with milk supply once your period returns, we are just a call away!
Don’t let milk supply or feeding struggles cause stress for you or your baby! At each lactation appointment, our lactation consultants complete a full oral assessment, discuss feeding patterns, take a full history on your milk supply, and offer strategies for boosting your milk supply once your period has returned. Book a one-on-one lactation consultation today
SDBFC is committed to providing high-quality lactation and functional nutrition consultations to parents in San Diego and beyond. Explore our postpartum, prenatal, and functional nutrition consultations, take a breastfeeding class or attend a workshop.
About the Author
Robin Kaplan has been an IBCLC since 2009, the same year that she opened up the San Diego Breastfeeding Center. Robin was the founding host of the Boob Group podcast and published her first book, Latch: a Handbook for Breastfeeding with Confidence at Every Stage in 2018. Melding her passions for supporting lactating parents and holistic health, Robin finished her Functional Nutrition Certification in 2023. In her free time, she enjoys hanging out with her two teenage boys, hiking, traveling, weaving, cooking, and searching for the best chai latte.
We Were Not Meant to Mother Alone
A few months ago, we sent out a Call for Breastfeeding Stories. Our desire was to flood the Internet with beautiful breastfeeding stories of triumph, overcoming challenges and struggles, and positive outcomes, regardless of the total amount of milk a mom was producing. We are thrilled to share these stories with you, our readers, and hope that they offer support and inspiration for you, wherever you are in your breastfeeding journey.
Thank you to all of the mothers who submitted their stories! If after you read these memoirs you are inspired to submit your story, feel free to send it to RobinKaplan@sdbfc.com.
_____
Our first breastfeeding memoir is from Michelle
I booked at least 2 vacations for my maternity leave, all on airplanes. I was going to wear my baby everywhere, nursing her as we went along. I had the organic breast pads purchased, all the nursing tanks, and the most breastfeeding-friendly bottles, but of course I wouldn’t need those for at least several months. I would see Mamas nursing their babes at the beach and I would find myself staring as I daydreamed about my nursling that was to come. December 2013, my sweet baby girl arrived. She latched and we were a nursing team. 24hrs later I was told she was Coombs positive and her jaundice levels were high. She was sleepy, was losing too much weight and I needed to give her formula in a bottle. I cried lots of tears. "FORMULA? No way!", but I had no other options. Every time I fed her, and I wouldn’t let anyone else feed her. I felt awful and felt like I was letting her down. 7 days later I was told, "your daughter is failure to thrive". Queue more tears, more formula, more guilt, and not a lot of milk being produced from me.
A few months ago, we sent out a Call for Breastfeeding Stories. Our desire was to flood the Internet with beautiful breastfeeding stories of triumph, overcoming challenges and struggles, and positive outcomes, regardless of the total amount of milk a mom was producing. We are thrilled to share these stories with you, our readers, and hope that they offer support and inspiration for you, wherever you are in your breastfeeding journey.
Thank you to all of the mothers who submitted their stories! If after you read these memoirs you are inspired to submit your story, feel free to send it to RobinKaplan@sdbfc.com.
_____
Our first breastfeeding memoir is from Michelle
I booked at least 2 vacations for my maternity leave, all on airplanes. I was going to wear my baby everywhere, nursing her as we went along. I had the organic breast pads purchased, all the nursing tanks, and the most breastfeeding-friendly bottles, but of course I wouldn’t need those for at least several months. I would see Mamas nursing their babes at the beach and I would find myself staring as I daydreamed about my nursling that was to come. December 2013, my sweet baby girl arrived. She latched and we were a nursing team. 24hrs later I was told she was Coombs positive and her jaundice levels were high. She was sleepy, was losing too much weight and I needed to give her formula in a bottle. I cried lots of tears. "FORMULA? No way!", but I had no other options. Every time I fed her, and I wouldn’t let anyone else feed her. I felt awful and felt like I was letting her down. 7 days later I was told, "your daughter is failure to thrive". Queue more tears, more formula, more guilt, and not a lot of milk being produced from me.
Over the next month, my journey consisted of doctors’ visits, pumping 8x a day, a baby screaming at the breast due to bottle preference and low supply, tube feeding, domperidone, and yet my milk never fully came in. 5 weeks in, a friend asked me to go to a breastfeeding support group. I went and hoped no one would notice me feeding formula to my sweet baby who wouldn't latch more than 5 minutes. Everyone noticed, yet no one judged me.
3 months in, at the Breastfeeding Support group that I now attended weekly, a Mama who I hardly knew asked if I wanted her to pump for me, and then another offered to help, as well. This would begin my donor milk journey, and a mental shift in my head that allowed me to stop seeing what I wasn't capable of, and start enjoying the beauty that came from a community that would end up feeding both of my babes! I threw away my pumping and tube feeding schedule right along with the lies that told me I wasn't enough because I couldn't get my body to do what I needed to do to fully feed my baby. We kept nursing as much as possible until 10 months and she got half formula and half donor milk.
A few months later, I was pregnant with my son. After my prenatal appointment at the San Diego Breastfeeding Center, I got permission from my doctor to start hand expressing at 37 weeks to collect colostrum to give my baby in the hospital through syringe feeding at the breast to help flush any jaundice he would have since he would be Coombs positive, as well. I started to collect donor milk and I had a community that donated enough breastmilk to supply him 9 full months as I only provided him about 30% of his needs with my own supply. He was born and I had a tiny bit more milk and a lot more confidence. I knew that no matter what, a nourished baby is a loved baby. I knew now that if I needed to give formula, I wasn't less of a mother. If I fed my baby pumped milk, donated milk, only could nurse a few times a day, used a cover, didn't use a cover, nursed for 3 months or nursed for 3 years, no matter what, I WAS ENOUGH. Even after a 6 day stay in the hospital for his Coombs, a tongue and lip tie revision, and a micro supply, we nursed for 10 months with donor milk through the SNS tube feeding at the breast. We then fed formula in a bottle and nursed as often as he wanted. He nursed until 16 months.
Today I am working towards my IBCLC, because of the non-judgmental support I received from the San Diego Breastfeeding Center community. They didn't sprinkle magic fairy breastfeeding dust on me that fixed all issues, but they gave me a plan that was doable. They gave me tools to accomplish the goals I set for myself. They gave me hope and they provided me with a community that was there to cheer me on. When I think about my breastfeeding journey, it is less about feeding my children, and more about the discovery that we Mamas cannot mother alone; we were never intended to do so. It takes a village to raise a baby, and for me, it took a village to feed mine. I am forever grateful.
Defining my Breastfeeding Experience: Inclusive Breastfeeding
Written by Aran Tavakoli
It has been nine months and I just put away my pump. Getting it ready for storage was bitter sweet. How many hours have I spent with that machine in the past 9 months? Its usefulness outweighed the annoyance. Once again, at this point in time, I am redefining my breastfeeding relationship with my baby.
Breastfeeding has been an extraordinary journey. I have experienced and learned so much. I keep searching for a word that captures and defines my experience, but I can’t find one. I believe the breastfeeding community is actually missing a term for mamas that fall into their own camp. There is the exclusively breastfeed group and the formula group. Research often distinctly divides mamas and babies into these two groups. But, there is an ever-growing group of mamas that breastfeed and give formula to support their breastfeeding relationship with their baby. The current words used to describe this group include combo feeding or more commonly, low supply needing supplementation.
Written by Aran Tavakoli
It has been nine months and I just put away my pump. Getting it ready for storage was bitter sweet. How many hours have I spent with that machine in the past 9 months? Its usefulness outweighed the annoyance. Once again, at this point in time, I am redefining my breastfeeding relationship with my baby.
Breastfeeding has been an extraordinary journey. I have experienced and learned so much. I keep searching for a word that captures and defines my experience, but I can’t find one. I believe the breastfeeding community is actually missing a term for mamas that fall into their own camp. There is the exclusively breastfeed group and the formula group. Research often distinctly divides mamas and babies into these two groups. But, there is an ever-growing group of mamas that breastfeed and give formula to support their breastfeeding relationship with their baby. The current words used to describe this group include combo feeding or more commonly, low supply needing supplementation.
From the true definition, I do not "exclusively" breastfeed my baby. However, I do exclusively give my baby all the breast milk that I have. But he needs more to be happy and healthy, so he also receives formula and when he was really little, he received donor milk. Honestly, I am so tired of the “low supply” conversation, I wish there was a different word for how I feed my baby. A word that matches the pride of the mamas who do exclusively breastfeed their little ones all that they produce.
Per Merriam-Webster, ‘exclusive’ is defined as, “not shared: available to only one person or group.” ‘Inclusive’ is defined as, “covering or including everything: open to everyone: not limited to certain people.”
Thinking about it, I have never been an exclusive type of person, so the opposite of exclusive is inclusive. I have inclusively breastfed my baby for 9 months (way longer than I would have thought in the beginning!). This is the word that I am using to define my breastfeeding experience.
In the inclusive camp, mamas know the best and worst of both worlds. The best of breastfeeding includes that joys of nourishing your baby with your body and making personalized milk. Then there is the best of formula: the intervention that provides life saving nutrition to support healthy growth and development. The worst of breastfeeding includes the sometime difficulties: mastitis, plugged ducts, yeast, blebs and so on! On top of breastfeeding, there might also be pumping, all the equipment and time that is required. For formula, besides the cost, the worst includes the bottles to be cleaned, sterilized and cleaned again.
In the inclusive camp, the mamas are incredible as they work so hard to maintain their milk supply for their little ones, while also accepting help in the form of formula or donor milk. It is not one way or the other, it is all the ways: the breastfeeding, the pumping, the supplementing, the love, the dedication, the tears and the sweat (especially on hot days)! The inclusiveness of the experience.
I don’t want to use a breastfeeding definition that makes mamas feel bad that their milk supplies are low (I worked through that one) or that they feel badly for needing to use formula (I worked though that one, too). Saying that, 'I inclusively breastfeed" is so much more positive and empowering than saying, "I have low supply and need to supplement." My lactation consultant, Ashley, always said to me, “He is getting your milk.” That has become my motto. He’s getting my milk, the amount doesn’t matter, and he is getting my milk.
So...Mamas who Inclusively Breastfeed, shall we adopt a new term?
Breastfeeding Misconceptions: Does Baby Weight Loss Mean Mom Doesn’t Have Enough Milk?
How many times have you heard a so-called ‘fact’ from a family member, friend, healthcare professional, or online resource that has your ‘mama-radar’ going off at warp speed? Maybe something just doesn’t sound right. Maybe it goes against all of your mama-bear instincts. Maybe it is completely contradictory to what you heard the previous day. Well, it’s time to start busting those myths and misconceptions!
Today, we start our new series called Breastfeeding Misconceptions.
Every month we will be BUSTING common breastfeeding myths and misconceptions, hopefully making your breastfeeding experience that much easier!
How many times have you heard a so-called ‘fact’ from a family member, friend, healthcare professional, or online resource that has your ‘mama-radar’ going off at warp speed? Maybe something just doesn’t sound right. Maybe it goes against all of your mama-bear instincts. Maybe it is completely contradictory to what you heard the previous day. Well, it’s time to start busting those myths and misconceptions!
Today, we start our new series called Breastfeeding Misconceptions.
Every month we will be BUSTING common breastfeeding myths and misconceptions, hopefully making your breastfeeding experience that much easier!
Myth #1: If your baby loses weight in the first week, it means your milk supply is low.
Not true!
All babies lose weight after birth:
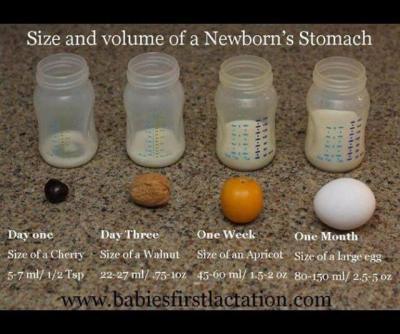
A newborn baby takes in approximately 5-7ml of colostrum per feeding in the first 24 hours. Babies are burning more calories than that as they attempt to breastfeed and expel that sticky, gooey meconium. Nature has provided the perfect amount of colostrum in those first few days to nourish your baby and while the quantity is small, the quality is jam-packed with every calorie, immunological property, protein, vitamin, and laxative that your newborn needs to poop and pee. Babies are expected to lose weight in those first few days. That doesn’t mean that mom’s supply is low.
Babies typically lose weight until mom’s ‘fuller milk’ comes in:
The amount of colostrum continues to grow as your milk transitions to ‘fuller milk’, which comes in around 2-5 days (depending on baby’s access to breast, effective sucking, birth interventions, etc.) Typical colostrum amounts are about 5-7 ml per feeding in first 24 hours, 7-15ml per feeding from 24-48 hours, and 22-27ml per feeding from 48-72 hours. Your baby will most likely lose weight until your ‘fuller milk’ comes in, but that doesn’t necessarily mean that you don’t have enough milk. What parents want to look for is that their baby is peeing and pooping (at least 1 of each per day of life) and baby’s weight loss plateaus once mom’s fuller milk has come in.
Here’s a great graphic of a baby’s stomach from Babies First Lactation and Education
Delayed milk supply doesn’t equal low milk supply:
There are several situations where a mother is at a higher risk for a delayed milk supply. As mentioned in this Best for Babes article, there are a number of factors that increase a mother’s risk for delayed milk supply. Some are beyond our control (or difficult to control): diabetes, obesity, thyroid problems, hypertension, PCOS, preterm birth, and anemia. There are also factors related to birth that can influence when a mother’s fuller supply comes in: cesarean birth, receiving lots of IV fluids, prolonged pushing stage, stress, cascade of interventions, hemorrhaging, mother-baby separation, just to name a few. If you are at a higher risk for having a delayed milk supply, it can be very helpful to speak with a lactation consultant within the first 24 hours after your baby is born. She can teach you ways to hand express and pump to help speed up the process of your fuller milk coming in, thereby DECREASING your risk for a low milk supply.
Lots of fluid during labor can cause greater weight loss in babies:
Studies have shown that mothers who have long periods of birth interventions (epidural, Pitocin, eventual emergency cesarean, etc.), tend to have more fluids during labor, thereby inflating baby’s birth weight and causing a large drop in baby’s weight in the first 24 hours. In those first 24 hours, we are looking for 1 pee and 1 stool (as a minimum.) For those babies that pee and stool multiple times in the first 24 hours, their weight loss is going to be greater, but that is not an indicator that mom’s supply is low. It just means they had a lot of fluids to expel after birth. Here are a few articles that explain this phenomenon. Dr. Jen: Newborn Weight and The Boob Group: Birth Interventions and Their Impact on Breastfeeding.
Baby may lose weight (or gain weight really slowly) because they are having a difficult time transferring mom’s milk:
There are many reasons why a baby might lose weight, sometimes continuing past the first week of life, even when mom has a full supply. Some of these include: engorgement (causing baby to have difficulties latching on), tongue-tie or lip tie, baby is recuperating after a difficult labor, baby is jaundiced, premature baby, etc. Again, when baby is losing weight due to these situations, it doesn’t always mean that mom’s supply is low. If her baby is having a difficult time transferring milk, then she should definitely meet with a lactation consultant to make sure she is doing everything she can to protect her milk supply until her baby can start to efficiently transfer milk from her breast.
Supplementation doesn’t equal formula:
If your milk supply is delayed, if your baby has elevated bilirubin, if your baby has lost more than 10% of his/her birth weight, that doesn’t automatically equal FORMULA supplementation. Mom may actually have enough of her own milk to supplement her baby with until baby’s weight is back on track. All she has to do is hand express or pump and see what extra she has. If mom doesn’t have enough of her own milk to supplement, then the hand expression or pumping (in addition to breastfeeding) will help to bring in her milk supply more fully. In the meantime, moms have other options. A mom can use milk bank breast milk or donor milk, if she prefers. For terrific information about milk banks, check out Human Milk Banking Association of North America and for milk sharing, check out Eats on Feets. The most important take away of this all…. When supplementation is necessary, it is imperative for a mom to increase her breast stimulation to help bring in her supply more fully. When her baby is getting a supplementation from another source, it is saying to mom’s body that she doesn’t have to make that amount of milk, which is totally not the case. The sooner mom’s fuller milk comes in, the sooner supplementation can decrease, so spend the extra time and effort… it will be worth it in the end.
Important note: When you might become concerned about your milk supply
While all of the above statements should illustrate why a mother should not be told that she has a low milk supply early on, there are some situations that might indicate that mom has a low milk supply (either temporarily or more long term.) If you are experiencing any of these situations, please connect with an IBCLC as soon as possible, as sometimes this can be a very temporary situation, as long as measures are taken quickly to protect mom’s milk supply. Here are some indicators that mom’s supply might be low:
Breasts did not grow and/or areola didn’t get darker during pregnancy
Breasts don’t feel heavier or fuller by 5-7 days postpartum
Fuller milk hasn’t ‘come in’ by 5-7 days postpartum
Baby is continuing to need supplementation to gain weight and mom is not making enough to supplement with her own milk
Mom has insufficient glandular tissue
Creating a Sense of Community When Using Donor Milk
In an effort to demystify milk sharing, for the next few weeks we will be sharing stories from breastfeeding moms who either donated their excess breastmilk or supplemented their baby with someone else’s milk. For more information about milk sharing, both informal and through milk banks, please visit our article: Supplement Options: Donor Milk, Milk Banks, and Formula, as well as our Boob Group podcast episode, Low Milk Supply: Donor Milk, Milk Banks, and Formula.
Today on the San Diego Breastfeeding Center blog, I am honored to share Cara's story, which demonstrates how a sense of community can blossom through supplementing with and donating breast milk. If you would like to submit your story to be shared with our readers, please email me at robinkaplan@sdbfc.com. Thank you so much, Cara, for sharing your inspiring story with us! Your daughter is so lucky to have you as her mother!
In an effort to demystify milk sharing, for the next few weeks we will be sharing stories from breastfeeding moms who either donated their excess breastmilk or supplemented their baby with someone else’s milk. For more information about milk sharing, both informal and through milk banks, please visit our article: Supplement Options: Donor Milk, Milk Banks, and Formula, as well as our Boob Group podcast episode, Low Milk Supply: Donor Milk, Milk Banks, and Formula.
Today on the San Diego Breastfeeding Center blog, I am honored to share Cara's story, which demonstrates how a sense of community can blossom through supplementing with and donating breast milk. If you would like to submit your story to be shared with our readers, please email me at robinkaplan@sdbfc.com. Thank you so much, Cara, for sharing your inspiring story with us! Your daughter is so lucky to have you as her mother!
----------------------------------------------------------------------------------------------------
I feed my daughter a mix of my breast milk, formula and donated breast milk from 5 different women. Not only has donated breast milk benefitted my daughter's digestion and overall health, it has introduced me to other moms that I'm now proud to consider part of my community.
We were only two days postpartum, after a beautiful unmedicated birth, when the first hospital-based lactation consultant looked at my breasts and her face fell a little bit. She informed me with a matter of fact tone that I might have breast hypoplasia/Insufficient Glandular Tissue (IGT). She said not to try too hard or be too hard on myself, as physiologically I might never make enough milk for my daughter. It turns out, she was right. When my milk finally came in, my daughter only transferred 10ml per feeding - less than half an ounce. However, through herbal supplements, medication, and pumping after each feeding I've managed nearly 4 months later to increase that amount to 20-30ml per feeding, but that's another story for another time. Bottom line: I've only ever made 8-10 ounces of breastmilk a day, max. Not nearly enough for my daughter. So at 4 days postpartum, after my daughter's weight dropped too far and my milk supply was not increasing: my husband helped me begin supplementing with formula using a syringe and feeding tube at the breast. I was just relieved to have a plan, and as my daughter thrived I was grateful for formula and the nourishment it was offering my baby.
At 6 days postpartum we met with a local IBCLC. She guided us on how to continue trying to increase my milk supply, and in the meantime how much to supplement. And she also mentioned donor milk.
I originally brushed off the idea of donor milk. While it made sense since human breast milk is the best food for babies, it seemed like it would be awkwardly intimate to use another mother's milk, and I was also afraid of disease. My husband and I were not in a place to pay the high price for formal milk bank donor milk, and informal channels made me nervous. I was also clinging to the hope that all the work I was putting into making my own breast milk would pay off and I might someday be able to exclusively breastfeed. A few weeks later, however, I had to come to the painful realization that would never happen. I cried as I realized I would be supplementing my daughter’s diet with either formula or donor milk for the long-term.
So I began looking into donor breast milk. I checked out the Human Milk for Human Babies Facebook pages, but was too uncomfortable with the idea of taking milk from strangers, so I sent an exploratory email to the moms I know in the area, asking if they or anyone they knew had extra milk they could donate. Somehow breast milk from friends or friends of friends made me a lot more comfortable. I only sent that email to 6 other mamas, but one friend responded that her friend had some extra milk due to an oversupply. Another friend/co-worker responded that she herself was weaning her toddler, and had just stopped pumping at work. She offered to resume pumping once a day and donate that milk to us. I was blown away with gratitude - what a gift… but, also nervous. Do we trust other milk enough to feed it to our daughter? My husband and I made a decision together: to trust. We decided these moms were feeding this milk to their own babies, so we would choose to feed it to our baby as well.
I first accepted donated breast milk from my friend and co-worker. I supplied her with breast milk storage bags which she filled and labeled. For her it was very little milk, just 4 ounces or so a day, but for us and my young baby that was a significant amount. I was so grateful, and felt humbled. This was a gift I could never repay. I would normally be uncomfortable with this imbalance - accepting a gift I couldn't repay - but was willing to do anything for my baby. And my friend's attitude helped tremendously - she was so kind and sweet and seemed honored to give this gift to my baby. A few days later, this friend texted me asking if my daughter liked her milk. I laughed as she explained that it felt like she'd made a casserole for someone -- and wanted to know if she liked it! My daughter certainly liked her milk, and I texted her a picture of my daughter in a post-meal milk-drunk stupor with a happily full tummy. After all - that happily full tummy was the reason we were doing all of this.
The friend-of-the-friend was also incredibly kind, and we set up a time to pick up the milk from her. She made me comfortable by asking if we were OK with the two cups of coffee she has in the morning. Just her awareness of this issue made me feel she was a conscientious Mama aware of how her breast milk could affect her baby, and my baby. She did request that we not tell her husband - as he would be weirded out by it all. This honestly made me a little uncomfortable as I was so recently myself overcoming the 'weirdness' factor. But she also seemed honored to help out and with an oversupply was happy her milk was going to good use.
I then met a woman with oversupply at a breastfeeding support group. She was exclusively pumping and had repeated bouts with mastitis so was pumping far more than her daughter needed in a day. I picked up some donated breast milk from her - feeling comfortable because we'd met a couple times at group, and I knew she'd struggled to do her best for her baby. We laughed a bit sadly as we realized we were in similar conundrums. Both pumping all the time - me in an effort to build supply and her in an effort to stave off mastitis. She seemed happy to help my daughter, and I promised to provide her with replacement breast milk storage bags. Somehow - buying donor moms breast milk storage bags feels like I'm repaying them just a bit - or at least making it a bit easier for them.
By 8 weeks of age my daughter was thriving with about a quarter to a third of her diet coming from my breast milk, and the rest a mix of formula and donor milk. I was first afraid to tell my daughter's pediatrician that we were using donated milk. At my daughter's two month appointment I tentatively brought up donor milk - then quickly mentioned I was aware of the risks of contracting diseases and the like. Our pediatrician didn't seem fazed at all that I was using donated breast milk - and she even encouraged it. She brought up the fact that women with new babies have been tested for infectious disease during their prenatal care - so the risks are very low. She was very comfortable with us feeding my daughter donated breast milk, which made me even more comfortable myself!
I was also so grateful for the donated breast milk as it also seemed to help my daughter’s tummy, as she began struggling with constipation from the iron in formula. We switched formulas to a brand we thought was better and cheaper - double bonus. However, my daughter started straining to pass hard little pellets, and stopped eating as much. We were very concerned. We began to consider giving her apricot nectar to help her bowels and with the hope she would start eating enough again. However, before the fruit juice, I wanted to try one more thing - my friend/co-worker had just given us about 12 ounces of breast milk so instead of spreading that amount out over a couple of days, I decided to try feeding it to her all in one day to see if it helped her tummy. It did! It made me sad to realize formula was affecting her so negatively, but so happy to have a tool on hand - donated breast milk - to help my daughter gently. We switched back to a brand of formula we knew worked better for my daughter, but she still had sluggish bowels.
Having seen the benefit of breast milk on my baby's tummy I decided to give Human Milk for Human Babies a try - milk from strangers. This decision was also encouraged by an internet community I had found of other mamas with low milk supply - some of whom were exclusively feeding their babies with donated breast milk from many different mamas. I posted a request on the Human Milk for Human Babies Southern California page on Facebook. Immediately after posting I panicked realizing the post might go up on other people’s news feeds. While my husband and I had become comfortable with donated breast milk, and I was open about my low milk supply struggles with friends and family, I was NOT open about using donated breast milk. I just didn't want to have to defend our decision, when we had been a bit conflicted about it ourselves. I'm still not sure if it went up publicly or not, but I decided to only deal with it if someone brought it up. They didn't.
First a woman in Anaheim asked if I would make the 3-4 hour round trip drive up there to get breast milk from her. I decided I wouldn't. I wanted donated breast milk for my baby, but formula was working OK and I decided the time in the car in Southern California highway traffic was not worth it for me and my daughter. Then another woman private messaged me saying she was in the area, had never donated before, didn't have any diseases, only had small amounts of alcohol after her infant daughter goes to bed for the longest stretch between feedings, and had some frozen breast milk that was about to expire and needed to be used. Her message made me feel comfortable, and I messaged her back thanking her for her openness and explaining I had never accepted milk from a connection with a stranger on a website before. We decided to meet for the first time at a mall near me, as she was going to the Hollister nurse-in.
It felt kind of like a Craigslist sale, meeting this stranger to exchange goods, except without the financial component. I texted her telling her to look for a woman wearing a sleeping baby in a baby carrier (me)- then she walked up wearing her daughter in a baby carrier as well - and with a large cooler full of frozen breast milk. Her husband and older son were with her, but as we started talking breastfeeding and postpartum struggles they wandered away. She sort of smiled and said her husband had wanted to come with her to meet this stranger from the internet. We laughed and then I wondered: why the heck was I so willing to just go meet a stranger from the internet without anyone with me?! Minutes after meeting her I'd felt comfortable. She was a mama with plenty of breast milk who stored some up when her daughter was much younger - and as the frozen milk neared its expiration date, she didn't want it going to waste. We are both moms who knew breast milk was best for our babies, and both moms doing our best to provide what we can. We've stayed in touch, as she might have some more milk for us in the future as she easily pumps above and beyond her daughter's needs. Even if she doesn't, we are grateful for the gift she has given us.
Since then, I met another mom in a breastfeeding support group, also exclusively pumping and with more milk than her daughter needs. After meeting her a few times and running into her in my neighborhood, she insisted she could begin providing us with fresh breast milk every couple of days. I accepted. Once again, I felt comfortable as I knew she was doing the best she could for her baby and attending support groups for support. Since then I've enjoyed meeting up with her for walks as we compared the struggles of new mama-hood.
I still sometimes have fears of my daughter contracting a communicable disease - or imagine the horror of a donor realizing she has something she didn't know she had - but have decided that the benefits outweigh the risks. I'm not yet open with family about the fact that we're using donor milk. Perhaps that's an indicator that I'm still not 100% OK with it, but mostly I think it's because I just don't want to have to defend our decision. The heartbreak of low milk supply is something I've learned to speak rather matter of factly about -- but how we choose to feed our daughter is nobody’s business, but our own. Who we choose to involve in that decision (for example: our pediatrician, our lactation consultant) is just that - our choice. Perhaps over time I'll be more open about the donor milk that is helping to nourish my daughter -- writing up our experience like this is a start!
Thanks to my breast milk, donated breast milk, and formula my daughter is thriving. Thanks to donated breast milk I've gotten to know other moms in a new way and we've built a community I never even dreamed we'd have. I am just so grateful for this gift other moms have given my daughter!
Mustering Courage to Accept Breastmilk From a Friend
In an effort to demystify milk sharing, for the next few weeks we will be sharing stories from breastfeeding moms who either donated their excess breastmilk or supplemented their baby with someone else’s milk. For more information about milk sharing, both informal and through milk banks, please visit our article: Supplement Options: Donor Milk, Milk Banks, and Formula, as well as our Boob Group podcast episode, Low Milk Supply: Donor Milk, Milk Banks, and Formula.
Today on the San Diego Breastfeeding Center blog, I am honored to share Christine McCarty's story about how she mustered up the courage to ask a friend for extra breastmilk for her baby. If you would like to submit your story to be shared with our readers, please email me at robinkaplan@sdbfc.com. Thank you so much, Christine, for sharing your inspiring story with us!
---------------------------------------------------------------------------------------------------------------
My story starts several months ago, when my daughter was about 5 months. I have a friend who has Raynaud's disease and pumps constantly to continue to give her son the best nutrition she can. We were having a conversation about breastfeeding (as most of our conversations are about, lol) and she mentioned she produced 80-120oz PER DAY! A few weeks later I was off to see my favorite IBCLC frantic and in tears because for 2 days I had only pumped 1.5oz (from both breasts total, not individually) per pumping session at work. I remember hugging my lactation consultant, crying in her shoulder, telling her "I'm losing it, I'm losing my daughter's lifeline, I'm such a poor mom, I just can't keep up." After much reassurance, we got back on the right track, but I still had the issue that my production hadn't gotten back up to speed for the next day I had to go to work.
In an effort to demystify milk sharing, for the next few weeks we will be sharing stories from breastfeeding moms who either donated their excess breastmilk or supplemented their baby with someone else’s milk. For more information about milk sharing, both informal and through milk banks, please visit our article: Supplement Options: Donor Milk, Milk Banks, and Formula, as well as our Boob Group podcast episode, Low Milk Supply: Donor Milk, Milk Banks, and Formula.
Today on the San Diego Breastfeeding Center blog, I am honored to share Christine McCarty's story about how she mustered up the courage to ask a friend for extra breastmilk for her baby. If you would like to submit your story to be shared with our readers, please email me at robinkaplan@sdbfc.com. Thank you so much, Christine, for sharing your inspiring story with us!
---------------------------------------------------------------------------------------------------------------
My story starts several months ago, when my daughter was about 5 months. I have a friend who has Raynaud's disease and pumps constantly to continue to give her son the best nutrition she can. We were having a conversation about breastfeeding (as most of our conversations are about, lol) and she mentioned she produced 80-120oz PER DAY! A few weeks later I was off to see my favorite IBCLC frantic and in tears because for 2 days I had only pumped 1.5oz (from both breasts total, not individually) per pumping session at work. I remember hugging my lactation consultant, crying in her shoulder, telling her "I'm losing it, I'm losing my daughter's lifeline, I'm such a poor mom, I just can't keep up." After much reassurance, we got back on the right track, but I still had the issue that my production hadn't gotten back up to speed for the next day I had to go to work.
I was in the grocery store about to buy some formula when I thought of my friend and how she was complaining she was running out of freezer space. I immediately put the formula back on the shelf. I knew I had to do something, but nothing about giving my daughter formula felt comfortable, and I wanted to exhaust the only other option I thought I had… my friend! I had to think about how to approach her to ask her about using her milk because I wasn't sure how comfortable she would be with it, since there's such a huge stigma attached. I mustered up the courage and called her to ask her to discuss milk sharing with her husband and see if they were mutually comfortable with it.
My friend started crying and I was in shock! Had I offended her? Was she sorry for me and my low production rate? Was this the end of our friendship? No way! She said she was so honored that I would come to her to ask for help and this meant so much to her to be able to help our family and help my daughter! She talked it over with her husband that night and it was settled. They brought 180oz to my house the next day along with her medical testing she had gotten done throughout her pregnancy and all she had afterwards, along with her son's paperwork.
The funny thing is, after I had gotten her milk, I became a total milk maid! My production boosted SO much! I'm sure it was because I knew I had her milk to rely on and that took off all the pressure I had put on myself. I didn't even need to use her milk until I had to go out of town for a week for work when my daughter was 8 months old. This time she donated 300oz. My daughter drank and lived happily off of her milk while I was across the country and when I came back she latched right back onto me and we've been nursing beautifully ever since. Now at 9 1/2 months she's still sucking strong and we'll continue to support breastfeeding and milk sharing :)
Also, my friend now feeds two other families who's children are exclusively drinking her milk (no solids yet), as well as her own six month old son, WHAT A ROCKSTAR!!!