Breastfeeding Misconceptions: Does Baby Weight Loss Mean Mom Doesn’t Have Enough Milk?
How many times have you heard a so-called ‘fact’ from a family member, friend, healthcare professional, or online resource that has your ‘mama-radar’ going off at warp speed? Maybe something just doesn’t sound right. Maybe it goes against all of your mama-bear instincts. Maybe it is completely contradictory to what you heard the previous day. Well, it’s time to start busting those myths and misconceptions!
Today, we start our new series called Breastfeeding Misconceptions.
Every month we will be BUSTING common breastfeeding myths and misconceptions, hopefully making your breastfeeding experience that much easier!
How many times have you heard a so-called ‘fact’ from a family member, friend, healthcare professional, or online resource that has your ‘mama-radar’ going off at warp speed? Maybe something just doesn’t sound right. Maybe it goes against all of your mama-bear instincts. Maybe it is completely contradictory to what you heard the previous day. Well, it’s time to start busting those myths and misconceptions!
Today, we start our new series called Breastfeeding Misconceptions.
Every month we will be BUSTING common breastfeeding myths and misconceptions, hopefully making your breastfeeding experience that much easier!
Myth #1: If your baby loses weight in the first week, it means your milk supply is low.
Not true!
All babies lose weight after birth:
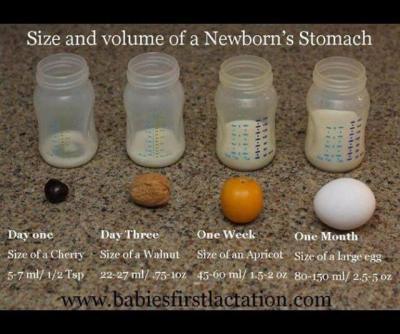
A newborn baby takes in approximately 5-7ml of colostrum per feeding in the first 24 hours. Babies are burning more calories than that as they attempt to breastfeed and expel that sticky, gooey meconium. Nature has provided the perfect amount of colostrum in those first few days to nourish your baby and while the quantity is small, the quality is jam-packed with every calorie, immunological property, protein, vitamin, and laxative that your newborn needs to poop and pee. Babies are expected to lose weight in those first few days. That doesn’t mean that mom’s supply is low.
Babies typically lose weight until mom’s ‘fuller milk’ comes in:
The amount of colostrum continues to grow as your milk transitions to ‘fuller milk’, which comes in around 2-5 days (depending on baby’s access to breast, effective sucking, birth interventions, etc.) Typical colostrum amounts are about 5-7 ml per feeding in first 24 hours, 7-15ml per feeding from 24-48 hours, and 22-27ml per feeding from 48-72 hours. Your baby will most likely lose weight until your ‘fuller milk’ comes in, but that doesn’t necessarily mean that you don’t have enough milk. What parents want to look for is that their baby is peeing and pooping (at least 1 of each per day of life) and baby’s weight loss plateaus once mom’s fuller milk has come in.
Here’s a great graphic of a baby’s stomach from Babies First Lactation and Education
Delayed milk supply doesn’t equal low milk supply:
There are several situations where a mother is at a higher risk for a delayed milk supply. As mentioned in this Best for Babes article, there are a number of factors that increase a mother’s risk for delayed milk supply. Some are beyond our control (or difficult to control): diabetes, obesity, thyroid problems, hypertension, PCOS, preterm birth, and anemia. There are also factors related to birth that can influence when a mother’s fuller supply comes in: cesarean birth, receiving lots of IV fluids, prolonged pushing stage, stress, cascade of interventions, hemorrhaging, mother-baby separation, just to name a few. If you are at a higher risk for having a delayed milk supply, it can be very helpful to speak with a lactation consultant within the first 24 hours after your baby is born. She can teach you ways to hand express and pump to help speed up the process of your fuller milk coming in, thereby DECREASING your risk for a low milk supply.
Lots of fluid during labor can cause greater weight loss in babies:
Studies have shown that mothers who have long periods of birth interventions (epidural, Pitocin, eventual emergency cesarean, etc.), tend to have more fluids during labor, thereby inflating baby’s birth weight and causing a large drop in baby’s weight in the first 24 hours. In those first 24 hours, we are looking for 1 pee and 1 stool (as a minimum.) For those babies that pee and stool multiple times in the first 24 hours, their weight loss is going to be greater, but that is not an indicator that mom’s supply is low. It just means they had a lot of fluids to expel after birth. Here are a few articles that explain this phenomenon. Dr. Jen: Newborn Weight and The Boob Group: Birth Interventions and Their Impact on Breastfeeding.
Baby may lose weight (or gain weight really slowly) because they are having a difficult time transferring mom’s milk:
There are many reasons why a baby might lose weight, sometimes continuing past the first week of life, even when mom has a full supply. Some of these include: engorgement (causing baby to have difficulties latching on), tongue-tie or lip tie, baby is recuperating after a difficult labor, baby is jaundiced, premature baby, etc. Again, when baby is losing weight due to these situations, it doesn’t always mean that mom’s supply is low. If her baby is having a difficult time transferring milk, then she should definitely meet with a lactation consultant to make sure she is doing everything she can to protect her milk supply until her baby can start to efficiently transfer milk from her breast.
Supplementation doesn’t equal formula:
If your milk supply is delayed, if your baby has elevated bilirubin, if your baby has lost more than 10% of his/her birth weight, that doesn’t automatically equal FORMULA supplementation. Mom may actually have enough of her own milk to supplement her baby with until baby’s weight is back on track. All she has to do is hand express or pump and see what extra she has. If mom doesn’t have enough of her own milk to supplement, then the hand expression or pumping (in addition to breastfeeding) will help to bring in her milk supply more fully. In the meantime, moms have other options. A mom can use milk bank breast milk or donor milk, if she prefers. For terrific information about milk banks, check out Human Milk Banking Association of North America and for milk sharing, check out Eats on Feets. The most important take away of this all…. When supplementation is necessary, it is imperative for a mom to increase her breast stimulation to help bring in her supply more fully. When her baby is getting a supplementation from another source, it is saying to mom’s body that she doesn’t have to make that amount of milk, which is totally not the case. The sooner mom’s fuller milk comes in, the sooner supplementation can decrease, so spend the extra time and effort… it will be worth it in the end.
Important note: When you might become concerned about your milk supply
While all of the above statements should illustrate why a mother should not be told that she has a low milk supply early on, there are some situations that might indicate that mom has a low milk supply (either temporarily or more long term.) If you are experiencing any of these situations, please connect with an IBCLC as soon as possible, as sometimes this can be a very temporary situation, as long as measures are taken quickly to protect mom’s milk supply. Here are some indicators that mom’s supply might be low:
Breasts did not grow and/or areola didn’t get darker during pregnancy
Breasts don’t feel heavier or fuller by 5-7 days postpartum
Fuller milk hasn’t ‘come in’ by 5-7 days postpartum
Baby is continuing to need supplementation to gain weight and mom is not making enough to supplement with her own milk
Mom has insufficient glandular tissue
Gerber to the Rescue (Or So They Want You To Think)
We’ve all been there.
You’ve been home with your new baby for a few days/weeks. It’s 2am and you’re tired and overwhelmed. You’ve never felt such bone-aching exhaustion. All you want to do is crawl in bed and sleep uninterrupted. Just for a few hours…. even ONE hour. But your baby is crying and won’t stop. You’ve tried everything – a fresh diaper, breastfeeding, you’ve shushed, swaddled and swung to the point of fatigue. And the baby won’t stop crying. You’ve woken your partner, called your mom or sister and none of the advice is helping. You’re worried that you’re doing something wrong or that you’re doing nothing right, that something is wrong with your little one, that you’re not making enough milk. You’d try almost anything at this moment to soothe your baby’s distress.
It’s exactly this vulnerability that formula companies prey upon when they make commercials like the one below:
The commercial for Gerber claims that the specially-created formula is effective in calming ‘excessive crying and colic.’ Nothing is more upsetting to a mother than the sound of her baby crying – we are biologically designed to physiologically respond to our own children’s sounds of distress, to do whatever we can to stop the baby from crying. Gerber is just PRAYING that a frustrated and exhausted mother will see this commercial and think that this new formula the answer to her struggles. Some moms may decide to introduce the formula to an exclusively breastfed baby, initiating the slippery slope of decreased supply and increasing ‘need’ for supplementation - just what formula companies are hoping for.
What Gerber fails to mention in the commercial is that the probiotic they have included (L. reuteri) has been studied and shown to exist in breast milk. Or that breast milk also has all the calories, protein, fat, carbohydrates and vitamins that your baby needs – AS WELL as antibacterial, antiviral, and antimicrobial factors specifically formulated to protect your baby. That breast milk contains all the probiotics AND prebiotics your baby may need. Or that human milk changes in composition as the baby grows, continually providing a unique superfood specific to YOUR baby.
Gerber also doesn’t explain to the new mom why her baby may be crying. The first three months of a baby’s life is often called the “fourth trimester” and should be treated as such. Just days ago, your baby was safely tucked in your womb, with constant warmth and soothing sounds and movements. Upon birth, the baby is thrust into his new environment, which is often cold and bright and always unfamiliar. Gerber doesn’t share the statistic that babies who are worn 3 or more hours a day cry 50% less than babies who aren’t. Gerber doesn’t remind the new mom that her 2-week old baby may be experiencing a growth spurtand the constant nursing and fussiness is a normal part of this, that the baby is doing all he needs to boost mom’s milk supply as he grows big and strong. Gerber doesn’t educate the mom on what she can add to or remove common allergenic or inflammatory foods (such as gluten, dairy, and soy) from her own diet to help soothe a colicky baby. (Check out our Boob Group podcast episode: GERD, Reflux and the Breastfed Baby for an explanation on symptoms, causes, and remedies for GERD, reflux, and colic.)
There are many reasons for a crying and colicky baby, and a number of solutions. One action that is never the answer is replacing any amount of breast milk with an artificial milk. Shame on Gerber for suggesting to an unsure and overwhelmed mother that her breast milk is lacking in something that could soothe her crying baby!
Finding My Tribe of Women Through Milk Sharing
Welcome to the World Breastfeeding 2013 Blog Carnival cohosted by NursingFreedom.org and The San Diego Breastfeeding Center!
This post was written for inclusion in the WBW 2013 Blog Carnival. Our participants will be writing and sharing their stories about community support and normalizing breastfeeding all week long. Find more participating sites in the list at the bottom of this post or at the main carnival page.
Welcome to the World Breastfeeding 2013 Blog Carnival cohosted by NursingFreedom.org and The San Diego Breastfeeding Center!
This post was written for inclusion in the WBW 2013 Blog Carnival. Our participants will be writing and sharing their stories about community support and normalizing breastfeeding all week long. Find more participating sites in the list at the bottom of this post or at the main carnival page.
***
This post was written by MJ Fisher.
Milk sharing has been a huge blessing in our lives! The mamas and families that have donated to us will forever have a place in our hearts and our lives. I believe using donor milk has impacted our breastfeeding relationship by saving it! I was not able to make all of my son’s milk, but so many awesome, generous mamas donated their milk to help feed our baby, which is a pretty amazing thing! Supplementing with donor milk motivated me to do everything I could to increase my supply and save our nursing relationship so I supplemented at the breast and nursed on demand. I’m super passionate and emotional about breastfeeding and milk sharing because I’m so extremely thankful our son has only had breast milk and also because he is 2 years old now and I’m still nursing him despite having a low supply.
When I was 23 years old with 38DD breasts, I had a breast reduction.... for good reasons, yes? Yes, but if I were to do it all over again, knowing that I could possible exclusively breastfeed, I think I might have waited on the surgery. But, then again, I might not have needed donor milk and met all my wonderful donor mamas!! I had my reduction in 1999 and my son was born in June 2011. After having an empowering homebirth, we had a few days of exclusively breastfeeding (EBF) bliss. Then our midwife weighed our son and he hadn’t gained enough and we were fighting jaundice. We got off cloud 9 and made a plan of what we needed to do – nurse, supplement, pump, supplement and repeat through the day and night. I wanted to nurse so bad and we only wanted our son to have breast milk so I opted to use a Supplemental Nursing System (SNS) with the donor milk. We nursed on demand, all day, during naps and throughout the night and supplemented with the SNS about 5 times a day in the beginning. It was draining, but I’m thankful now because I believe it only helped my supply. I’m also very lucky that my son was fine with any amount of milk I could make for him, I know some babies get frustrated when the milk doesn’t flow and mine did not when we nursed without the SNS.
Our midwives enlightened my husband and I (as they have done about a TON of things) about donor milk because we had NO CLUE! Even my sister, a post partum doula in LA, knew about milk banks and the decent amount of money they charge. Our midwives told us that there are mamas out there that make more milk than their babies need and they will donate it – my heart just dropped and tears were running down my cheeks, I still have no words! What a selfless act! Taking time out multiple times in your day, away from your children, to pump milk to feed other babies and help them to thrive and if you’ve ever pumped before you know what a PITA that can be! We had our hearts set on our baby only having breast milk, for we knew how beneficial it was to build a strong immune system, resistance to disease and infection, as well as many long term health benefits, so having milk donated to us was a huge stress reliever.
Now that we decided we wanted donor milk, we had to find it. It was always quite a journey, trying to find milk, not knowing if we would get enough, driving all over the county, sometimes out of the county to pick up milk. Meeting other mamas who helped us feed our baby for a one time encounter/donation or for the fourth or fifth time suddenly became our friends, with us even scheduling play dates with our kids. Sometimes my husband would make the milk run – we joked that he was my milk man! Thankfully we got a lot of donors sent our way from our midwives. They would give us a little background on the mama and we found comfort knowing they came recommended from them. We were so blessed to have had a few long term donors, one mama who pumped 45-50oz per day!!! When we would find donor mamas outside of our midwives (we used Eats on Feets Facebook page) there were a few questions our midwife gave us to have the donor answer. Since we had no connection with the mama, those questions helped us get to know her a little better and determine if she was a good match for us, our baby and our comfort level.
Here are the questions - Can you tell me a bit more about you? What’s your baby's age? Do you drink alcohol/caffeine? Where did you deliver, hospital or home? Can you tell me a bit about your diet? I presume no, but any diseases you are positive for?
I know some mamas that feel they don’t need to ask any questions and feel that if the donor mama breastfeeds her own baby then there is no need to worry about anything being wrong with the milk. For us, we liked to get to know the mama and it made us feel better when a donor mama didn't hesitate to answer any of our questions. I would hope she would put herself in my shoes and would do the same thing.
Our son has had about 10 different donors from birth to 1 year old. We'd like to think he's a super baby with so many different mamas' antibodies! I feel like we can never thank our donor mamas enough for helping us feed our baby and giving him the chance to be as healthy as possible with only breast milk. With the help of my midwives (also a LC), my husband, my donor mamas, the SNS and both me and my sons want to EBF we are still nursing at 2 years old!!! We supplemented with the SNS using donor milk until 12 months old. Then we used goat milk in the SNS until 18 months old. All of our hard work paid off when I finally became an EBF Mama! I feel like my supply improved with the use of the SNS and I never would have used the SNS if I didn’t have donor milk.
To put a cherry on this breastfeeding sundae, all of my donor mamas are now my friends. Some are my soul sisters, a part of the village of mamas I surround myself with to lift me up and cheer me on! This whole experience has enriched my life, my family’s life and given me peace with a decision I made to have surgery. Anything that is “worth” it, doesn’t come easy anyways!
One Breastfeeding Love,
Mj Fisher (Married to Jason, Mama to Jason Jr. ~ 2 years old)
***
Visit NursingFreedom.org and The San Diego Breastfeeding Center for more breastfeeding resources and WBW Carnival details!
Please take time to read the submissions by the other carnival participants. Below are a list of links for today's participants; you can find a complete list of links (updated throughout the week) at our main carnival page:
(This list will be updated by afternoon August 5 with all the carnival links.)
- An Unexpected Formula-Fed Attachment — Kyle (of JEDI Momster and) writing at Natural Parents Network, exclusively breastfed three healthy babies. So when she was pregnant with her fourth, she assumed she would have no breastfeeding troubles she could not overcome. Turns out, her fourth baby had his own ideas. Kyle shares her heartfelt thoughts on how she came to terms with the conclusion of her breastfeeding journey.
- It Take a Village: Cross Nursing — Shannah at Breastfeeding Utah shares how cross-nursing helped her baby in their time of need, and how that experience inspired her to create a community of cross-nursing and milk-sharing women.
- Random little influences and Large scale support communities lead to knowing better and doing better — amy at random mom shares how her ideas and successes involved with breastfeeding evolved with each of her children, how her first milk sharing experience completely floored her, and how small personal experiences combined with huge communities of online support were responsible for leading and educating her from point A to point D, and hopefully beyond.
- Mikko's weaning story — After five years of breastfeeding, Lauren at Hobo Mamashares how the nursing relationship with her firstborn came to a gentle end.
- My Milk is Your Milk — Lola at What the Beep am I Doing? discusses her use of donor milk and hhow she paid the gift back to other families.
- World Breastfeeding Week 2013 Blog Carnival - Celebrating Each Mother's Journey — Jenny at I'm a full-time mummy lists her experiences and journey as a breastfeeding mother.
- Working Mom Nursing Twins — Sadia at How Do You Do It? breastfed her twin daughters for 7 months. They made it through premature birth and NICU stays, her return to full-time work, her husband's deployment to Iraq, and Baby J's nursing strike.
- So, You Wanna Milkshare? — Milk banks, informed community sharing and friends, oh my! So many ways to share the milky love; That Mama Gretchen is sharing her experience with each.
- Milk Siblings: One Mama's Milk Sharing Story (and Resources)Amber, guest posting at Code Name: Mama, shares how her views on milk sharing were influenced by her daughter receiving donor milk from a bank during a NICU stay, and how that inspired her to give her stash to a friend.
- Humans Feeding Humans — Krystyna at Sweet Pea Births shares ideas on how we can celebrate all the different ways modern mommies feed their babies. While we are comfortable with the breastmilk-formula paradigm, she proposes that we expand our horizons and embrace all the different ways mamas feed their infants.
- When Breastfeeding Doesn't Go As Planned — MandyE of Twin Trials and Triumphs shares the challenges she faced in feeding her premature twins. She's still learning to cope with things not having gone exactly as she'd always hoped.
- Taking Back My Life By Giving Away My Milk — When Amanda Rose Adams's first child was born, he was tube fed, airlifted, ventilated, and nearly died twice. In the chaos of her son's survival, pumping breast milk was physically and mentally soothing for Amanda. Before long her freezer was literally overflowing with milk - then she started giving it away.
- The Tortoise and the Hare — Nona's Nipples at The Touch of Life discusses why we care about breast milk and formula with everything inbetween.
- Finding My Tribe of Women Through Milk Sharing — Mj, guest posting at San Diego Breastfeeding Center shares her journey breastfeeding with low milk supply and supplementing with donor milk using an at the breast supplemental nursing system. She shares the impact milk sharing has had on her life, her family, and how it saved her breastfeeding relationship. Her article can also be found at her blog:
- Human Milk for Human Babies — Sam at Nelson's Nest shares her perspective on milk-sharing after an unexpected premature delivery left her pumping in the hopes of breastfeeding her son one day. Sam's milk was an amazing gift to the other preemie who received it, but the connection was a blessing in the donor mom's life too!
- Sister, I Honor You — A mother feeding her baby is a triumph and should be honored, not criticized. Before you judge or propagate your own cause, go find your sister. A post by Racher: Mama, CSW, at The Touch of Life.
- Every Breastfeeding Journey Is Different, Every One Is Special — No two stories are alike, evidenced by That Mama Gretchen's collaboration of a few dear mama's reflections on their breastfeeding highs, lows and in betweens.
- Quitting Breastfeeding — Jen W at How Do You Do It? share a letter she wrote to her boys, three years ago exactly, the day she quit breastfeeding after 9 months.
- A Pumping Mom's Journey — Shannah at Breastfeeding Utah shares about her journey pumping for her son, who was born at 29 weeks.
This InLinkz account has expired. You can still view the linkup here
Breast Friends
Welcome to the World Breastfeeding 2013 Blog Carnival cohosted by NursingFreedom.org and The San Diego Breastfeeding Center!
This post was written for inclusion in the WBW 2013 Blog Carnival. Our participants will be writing and sharing their stories about community support and normalizing breastfeeding all week long. Find more participating sites in the list at the bottom of this post or at the main carnival page.
***
This post was written by Mama Bree.
After a couple days of moving down the birth canal with each surge, and balancing between two worlds, I made my beautiful entrance and planted myself firmly (and loudly) on this side of the womb. My tiny body and mind were bombarded with so many new sensations. My temperature was cooler, I could create sound, the dim lights were still much brighter than I had ever seen...and there was love. I was instantly placed on my mommy. My daddy's hands rubbed me. They kissed me and I could clearly hear the voices that had become so familiar.
Welcome to the World Breastfeeding 2013 Blog Carnival cohosted by NursingFreedom.org and The San Diego Breastfeeding Center!
This post was written for inclusion in the WBW 2013 Blog Carnival. Our participants will be writing and sharing their stories about community support and normalizing breastfeeding all week long. Find more participating sites in the list at the bottom of this post or at the main carnival page.
***
This post was written by Mama Bree.
After a couple days of moving down the birth canal with each surge, and balancing between two worlds, I made my beautiful entrance and planted myself firmly (and loudly) on this side of the womb. My tiny body and mind were bombarded with so many new sensations. My temperature was cooler, I could create sound, the dim lights were still much brighter than I had ever seen...and there was love. I was instantly placed on my mommy. My daddy's hands rubbed me. They kissed me and I could clearly hear the voices that had become so familiar.
Then, a new feeling: hunger came over me and I began the journey to find sustenance. Using instinct, my awesome sense of smell, and a little adult help, I found my mom's breast and latched on with ease. I filled my tiny belly and found immence comfort against my mommy's heart.
Shortly after my early morning meal, we fell asleep as a family. We rested that way for the whole first day. On the second day, we had visitors. Family and new friends filled our room and it overflowed with joy, love and some take-out meals for my parents.
On the third day we headed towards my new home. I was dressed for the first time and placed in my "Adventure Seat". The nurse gave us a thumbs up and wished us well, but the doctors were worried about my new belly button. In a blink we were moved to a new area. This area was different. There were bright flashing monitors, tubes, alarms, and there was sadness and hope all swirled together. My mommy was crying. Daddy was talking and asking questions. And I was getting poked, taped, and placed in a bed alone with wires attached.
I felt the need to be close to my mom. I wanted her to hold me to her heart and fill my belly. I was scared. She was scared too. She couldn't hold me at first, but as soon as she could she scooped me up. I was really hungry then! I was frantically trying to attach to my mom. It was much harder than it had been before we moved to this new place. I could feel tightness and fear. We struggled to find the rhythm we had created in our birthing room. After several hours and a couple dry diapers the nurses insisted on feeding me by any means necessary. They told my mom that her supply was not enough and I was too hungry to wait for it to come in.
Safety seals were popped and a tube was placed on a finger. I ate, but there was no heart.
After only 2 days of monitoring I was allowed to return to a private room with my mommy and daddy. Though my belly button was no longer a concern, nursing did not improve. I was hungry and unable to fill my belly. My mommy spent hours pumping, trying to get me the milk I needed. She was so sad. I could feel her disappoint and sorrow. My daddy struggled to help us both feel better, but we couldn't.
We left the hospital on the 5th day of my life in this world. My mommy was armed with a nipple shield and daddy carried out tubes, formula, and syringes. I could tell that I was hurting my mommy when I tried to eat. We were both struggling.
The following day was a Wednesday. I was 6 days old when daddy insisted and dropped us off at a breastfeeding group. As we entered, my mommy started crying. There were so many women and it was a little overwhelming. The Lactation Consultant greeted us and rubbed mommy's back while she gathered herself. It was that moment that our breastfeeding path was forever changed. We sat next to a young mommy and her daughter. They had also supplemented formula and finger-fed. I felt my mommy relax as she found solidarity in the ladies around her. Everyone was encouraging. Everyone talked of solutions. Everyone was kind.
All around that room were mommies and babies of all ages. Babies were sleeping peacefully or nursing happily. Even those struggling, like us, seemed to be on the path toward pain-free --even pleasant nursing. Though I slept the entire time that first day, my mommy got some wonderful advice and recommendations that we implemented immediately and found some much needed relief.
We returned to that group every Wednesday, week after week. We delighted in meeting new mommies. We formed friendships. Strong friendships, with strong, beautiful women and sweet, beautiful babies. My mommy calls them her "Breast Friends".
We continued to meet every Wednesday, long after we truly needed breastfeeding support, so that we could now offer support to other moms. That first Wednesday my mommy NEEDED to see all of the older babies nursing successfully for her to attempt to be successful nursing me. If these bright and loving women--who all had some struggles-- were breastfeeding blissfully, then so could we. Period. We wanted to be there every week as a representation of blissful breastfeeding, but mostly we wanted to be there to encourage anyone that was having a hard time, anyone who could use a smile, some fellowship, or maybe just a rub on the back.
I've been laying against my mommy, filling my belly to the beat of her heart for 9 months now. We have no intention of stopping, even as I discover newer and more solid foods. We had some ups and downs, but made some lifelong Breast Friends in the process.
I often hear my mommy say that every mommy needs Breast Friends. You need people who are going through the exact same stuff as you at the same time --the joys and the struggles! You need an outlet to freely discuss the frequency and color of your baby's poop and people who genuinely care about the condition of your nipples. Every mommy needs Breast Friends and we were so blessed to find ours at our Wednesday Breastfeeding Group.
***
Visit NursingFreedom.org and The San Diego Breastfeeding Center for more breastfeeding resources and WBW Carnival details!
Please take time to read the submissions by the other carnival participants. Below are a list of links for today's participants; you can find a complete list of links (updated throughout the week) at our main carnival page:
(This list will be updated by afternoon August 1 with all the carnival links.)
- If You're Worried About Your Kid Seeing Me Breastfeeding, You're Doing It Wrong — Dionna at Code Name: Mama is living the breastfeeding-as-a-cultural-norm dream. She has first-hand experience that kids, teens & adults who seebreastfeeding accept breastfeeding.
- Supporting Breastfeeding Online — Wendy at Breastfeeding Utah reaches out to birth and breastfeeding support professionals who are interested in knowing more about supporting their clients online.
- Breast Friends — Mama Bree, guest posting at San Diego Breastfeeding Center, shares a baby's journey to blissful breastfeeding with a little help.
- World Breastfeeding Week 2013 Blog Carnival - Online Breastfeeding Support — Other than buying and reading up on books, Jenny at I'm a full-time mummy finds that it is useful to read up on other mums’ breastfeeding experiences and how they deal with their obstacles.
- It Takes a Village... — Meredith at Thank You Ma'am talks about the support she got from her family, especially from her own mom, who is a lactation consultant.
- Community Support — Ashley at ModerationMama tells about her supportive community surrounding her breastfeeding journey, and she talks about the importance of the breastfeeding class she took while still pregnant.
- Finding a Nanny to Be Part of My Village — Before returning to work, Gretchen of That Mama Gretchen, posting at Natural Parents Network, needed to find a trusted caregiver for her daughter. Someone who supported her parenting goals and was ready to become part of a family.
- A Nursey Love Letter — When asked about her nursing support group, KassK of Get Born Tribe surprised herself with the answer: her husband!
- We are mammals. — To be a mammal . . . what does that mean? Practicing Mammal educates us.
- Building a Solid Foundation for a Successful Breastfeeding Journey — Tia at Tia's Sweeps Go 'Round shares how she built a strong support network to help her successfully breastfeed her newborn daughter.
- Stubbornness and Support: My Breastfeeding Journey — Diana at Munchkin's Mommy shares her breastfeeding journey, from unhelpful nurses to a gentle guide, and her sheer stubbornness.
- Looking online for breastfeeding support — The author at "Just" A Mom has found many ways to use the internet to support her mothering and breastfeeding journey, and she has learned how to keep her online experiences positive.
- The Village that didn't feed — Nona's Nipples at The Touch of Life explains how our communities influence our choices. She explains how she came to breastfeed and how it was taken away.
- Nursing By Example — Krystyna at Sweet Pea Births decided to nurse through a pregnancy and to try tandem nursing thanks to the support from her La Leche League leader and another mother in her community. Read about the resources that were helpful and the lessons she learned on her journey into tandem nursing.
- A Burden Shared: How my IBCLC Lightened my Load — My IBCLC rocks!! smscott at In All Things...One Step at a Time's journey would not be possible without a huge contribution of time and energy from her IBCLC. Her difficult times were measured in weeks and months instead of moments.
- Fathers Need Breastfeeding Support Too — Destany at They Are All of Me recalls that the biggest detriment to her breastfeeding success was her husband's strong disapproval.
- Breastfeeding Support Over the Years — Valerie at Momma in Progressdiscusses the range of support she received over her seven-year breastfeeding journey.
- Uncharted Territory: Breastfeeding — Michelle at Oh, The Simple Joys describes her change of heart regarding breastfeeding and the kind souls who helped along the way. From thinking formula was the norm to extended ecological breastfeeding, this is her story. Her story also includes breastfeeding after a hospital birth, dealing with inverted nipples, and the lactation consultant who helped to name her daughter.
- Online Breastfeeding Support: Finding Success, Acceptance and Friendships — Author and CLEC Lara Audelo of Virtual Breastfeeding Culture shares how online breastfeeding support changed her entire life, and why so many mothers are drawn to it, rely upon it, and place such value on their virtual mother-to-mother connections.
- Staying Connected---Online Breastfeeding Support for AD Military Moms — Breastfeeding in Combat Boots shares how important online support is to the success of breastfeeding for mothers serving in the military.
- Breastfeeding and Community — Amy W. at Me, Mothering, and Making it All Work discusses ways in which community affects breastfeeding dyads and makes suggestions for accepting and supporting nursing as normal and necessary.
- World Breastfeeding Week 2013 Blog Carnival - Community Support — Jenny at I'm a full-time mummy has been breastfeeding NON-STOP since 4th March 2009, the day her first child Benjamin was born. Jenny shares who has been in her community of breastfeeding supporters.
- Oversupply as a Blessing in Disguise: Milk Sharing and Wet Nursing — Tooele Birth and Breastfeeding, guest posting at Code Name: Mama, tells how she ended up donating breastmilk and wet nursing several babies. She shares the benefits from both a recipient and a donor.
You can still view the linkup here
Help a Mama Out: Overcoming Nursing in Public Anxiety
‘Help a Mama Out’ Topic of the Week: What are your favorite tips for overcoming anxiety about breastfeeding in public?
Sandy: Take along a support person
Melanie: Practice in front of a mirror. Another thing that helped me was to just focus all of my attention on my baby. I learned not to look around for a reaction from a stranger.
Miranda: Bring a light shawl to cover up, and remember, you are protected by law to breastfeed in public!
Marie: Have someone with you who is either a) also nursing and has no issues nursing in public or b) is super supportive of you nursing in public. Also, the first couple of times, go somewhere you are already comfortable, like a local bookstore or Starbucks.
Sara: So whatever makes you most comfortable! Practice, practice, practice! So it in front of people you are comfortable with first, then adjust slowly. Find your comfort zone and be happy with it.
Kat: I started going to places and having play dates with other moms who nursed in public.
Keep Austin Nursing in Public: Check out The Badass Breastfeeders free e-course: Becoming a Badass Public Breastfeeder. Know your rights (breastfeedinglaw.com). Surround yourself, even if it’s only online, with a support system. Breastfeed in a bubble… I never pay much attention to those around me when I’m nursing. I’m not looking around for real or possibly imagined dirty looks or sideways glances.
KC: I wore a nursing tank with a t-short on top. Undo the tank from the top and lift your shirt up from the bottom and use that to shield yourself until baby latches. Then the shirt just rests on the baby’s cheek. Second he popped off, I pulled my shirt down and fixed the tank from the top. It helped me feel like I wasn’t exposing everything to everybody. My friends called me the ‘stealth nurser’ because no one knew I was nursing.
Lisa: Practice in a breastfeeding support group. Also, just do it and your comfort level will increase over time.
Raquel: Try practicing breastfeeding in a carrier. I nursed all 3 of my kids in my ergo. Not only was I hands free, but no one was the wiser when I had the little sleeping hood over their heads.
Marybeth: Take a buddy – someone who will talk to you, smile and chat with you, and treat you like it’s normal (it is!!!) while you tackle your anxiety.
Amanda: Start gradual. Start in your car with a cover. Move to a quiet out of the way corner. Eventually, you’ll just get rid of the cover (because your baby will hate it!) and feed anytime, anywhere. I have Momzelle shirts, but you can easily make your own as well. Keeps my tummy covered and lets me feed discretely.
Brooke: A deep v-neck shirt works great to pull your boob up and out….LOL!
Michelle: I use a muslin blanket when I’m out. It’s nice and cool and you can tuck it into your bra strap for security. You’ll be rocking NIP in no time!
Natural Parenting: Just start. It may be awkward at first, but the more you do it, the easier it gets. Also, what helped me was to nurse uncovered in front of a mirror at home – once I saw in the mirror what everyone else saw (i.e. how little flesh is really exposed), it made it a lot easier for me.
Stephanie: This video says it all
Help a Mama Out: Surviving Your Baby’s Witching Hours
‘Help a Mama Out’ Topic of the Week: What are Your Best Tips for Surviving Your Baby’s Witching Hours?
Ashley: Wearing the baby during the evening hours. Prepping dinner earlier in the day so that I didn’t have to do it during my baby’s fussy time. Setting aside special activities for my then 3-year old that she could do on her own or with little help from me, just in case I needed to be sitting on the couch, constantly nursing the baby. Reminding myself that this was temporary and would pass!
Karen: Feeding a little at a time, more frequently. I read when #4 had HORRIBLE colic that there are some cultures where babies never experience colic. In all of these communities, babies are worn and are on and off the boob all day, so they eat small meals very frequently.
Kat: Support from my husband was really crucial during this time. I would nurse my son and concentrate on him while my husband got dinner ready. Holding and wearing baby helped the most. Also, fresh air worked wonders!
Lori: Babywearing…. I would also batch cook on the weekend when Daddy was home so that come dinner time, all I had to do was heat it up.
Catie: Remain calm…. Baby seemed to sense the angst and it only made things worse. Often baby and I both needed a breather. My husband was deployed when my son went through the worst of it so handing him off wasn’t an option. I would set him down in a swing or bouncy chair with a toy, walk to another room and take 30 seconds minimum to breathe, drink some water, etc. If baby was happy, I took a break away from him since we were obviously over-stimulating each other. Then, back to nursing, rocking, wearing, walking, etc…. until we could both get a good nap!
Janina: Babywearing, smaller feedings, burp a lot, white noise, gripe water at the first sign of crying, rocking, and time.
Christina: Wearing and then walking – close to mom, plus amazing fresh air and rhythmic movements. Sometimes getting into a warm bath with my daughter helped, too.
Shelly: Lowering my expectations. Fussy babies meant nothing was getting done except baby care. Going for a walk helped clear my head and the change of scenery almost always calmed them down.
Kathryn: Bouncing on the exercise ball and the vacuum was a lifesaver.
Grace: Adjusting my diet (cutting out gluten and dairy because those were his colic culprits). Make the day less chaotic by staying home or no visitors, low lights, soothing music. Skin to skin. Take a warm bath with baby on my chest. Baby massage with some coconut oil and lavender oil. Colic Calm if it lasts more than an hour.
Turath: Our baby’s witching hour turned out to be a dairy sensitivity, so after I cut out dairy we haven’t had any problems. Definitely babywearing! This article has lots of great tips…. It’s sleep related, but I think many of the tips will work for calming a fussy baby. http://www.askdrsears.com/topics/parenting/fussy-baby/31-ways-get-your-baby-sleep-and-stay-asleep
Rhianna: Try putting them to bed earlier. Once we instituted a 6pm bedtime, it was MUCH easier!
Kenyatta: Wear them! Familiarity (routine, music, lighting, smells) and calm.
Here are a few of my favorite articles:
A Checklist of 36 Time-Tested Baby Calmers
The Phenomenon of Late Afternoon/Early Evening Infant Crying: Part 1
The Phenomenon of Late Afternoon/Early Evening Infant Crying: Part 2
Help a Mama Out: Weaning a Toddler
Weaning a toddler can be a struggle and can come along with a lot of emotions. Get our team’s best tips for weaning a toddler in this “Help a Mama Out” article.
‘Help a Mama Out’ Topic of the Week: Tips for Weaning a Toddler
Kelly: Take it slow and take cues from your toddler. We haven’t completely weaned yet, but in order for ME to keep our breastfeeding relationship in a good place, I had to take is down to 3x a day. While I wanted to distract and push away when the little one wanted to breastfeed, what he really needed was a few minutes of cuddling before he was on to the next thing. Once I figured that out, taking it down to 3x a day was a breeze and I feel like I could do this forever now (or at least until HE wants.)
Heather: Honestly, let the toddler decide when to wean. That is what I plan on doing with my daughter. She is 18 months and still nursing strong!
Heidi: Sit them down and have a little heart-to-heart – worked with both of mine! It’s incredible how much they really ‘get it.’
Lolis: I got pregnant! Just cut out feedings by distracting her. Nursing is a two-way relationship and if you don’t want to do it anymore, then your feelings should be respected, too. I thought I would end up tandem nursing, but she weaned when I was 30 weeks pregnant and has tried a few times since then, but I just distracted her to take her mind off of it. I’ve said ‘no’ a few times, too. Try to also offer a drink when they are trying to nurse because sometimes they are just thirsty. I also wear shirts that make the boobies inaccessible. We made it to 21 months and I’m completely ok with that.
Theresa: When my daughter was a little over 2 years old I became pregnant and nursing was suddenly very uncomfortable for me. We took weaning very slowly and gradually, cutting it back to naptime and before bed. We had lots of honest talks about how mommy’s body was changing and that nursing was uncomfortable for me (not that she hurt me) because of those changes. I incorporated giving her a cup of unsweetened coconut milk before going to bed as ‘big girl milk.’ I really emphasized how special our snuggle time was to me and reassured her that it wouldn’t stop just because she wasn’t having mommy milk anymore. It took several months and, to be honest, a few teary times for both of us. She breastfed for the last time when she was 32 months and started referring to it as ‘baby milk’ instead of ‘mommy milk.’ Also, once I stopped nursing, I switched from wearing nursing tanks to a bra and T-shirt. It seemed to make it easier for her to accept a gentle ‘I can’t. Mommy is not wearing the right type of shirt,’ on the random times when she still wanted to try.
Susan: Just finished weaning my 15 month old and low supply played the biggest role. Once those first few days of sadness was over (for me), it was a relief to know she was happy as a clam getting a full 6-8 oz of non-dairy milk and I felt great knowing she is healthy and thriving. I’ve realized we all take a different path in this motherhood and nursing thing and we all do what we can for the well-being of our children. I totally agree with Lolis that nursing must be a mutual two-way enjoyable experience and if mommy is done that must be respected as well.
Adrienne: Having specific times of the day for nursing helped us. We loved first thing in the morning, naptime, and bedtime. Then I could say ‘not now, but we can nurse at naptime.’ This made her actually ask to go to bed. Of course, there were exceptions for major physical and emotional injuries, but this worked for us. Distraction, staying busy, avoiding places that reminded her of nursing, offering something else instead (like a book, snack, drink, cuddle, etc.) also helped.
Donna: I use distraction as much as possible and tell him that they are empty when they are. Eventually they forget and nursing is replaced by cuddles J
Kathy: ‘Don’t offer, don’t refuse’ worked best for me and my son. Shortly after his second birthday, he just stopped asking one day. Seems like a lifetime ago and I miss it!
Don't miss our Boob Group podcast episode: Breastfeeding Toddlers: Night Nursing and Weaning
Here are a few more articles on weaning and toddlers on our blog:
Gentle Weaning: What is the Process?
Gentle Weaning: Techniques and Resources
Help a Mama Out: Getting the Most Milk Out While Pumping
Alison: Massaging the breasts! That’s the biggest helper for me. Also, leaning over a bit, as gravity can sometimes help.
Nova: Crank it up if you can tolerate it. If your pump has those little white membranes, change them once a month or so.
Sondra: Relax!
Melissa: Whenever I pump at work, I put a little coconut oil on the inside of the pump flanges. This way the inside is lubricated and my areola doesn’t chafe alongside of the plastic flanges.
Laura: If I need to increase volume, I get into a pumping boot camp and spend an hour pumping with 10 minute intervals and 10 minute breaks. Whenever I have a supply dip, this would bring it back within a day or so. Also, I’ve had great output when I watch a comedy where I am laughing out loud. And it never hurts to have my hubby give me a back massage just before pumping or during a break. Also, my supply is related to my water intake, so I make sure to drink a minimum of 100oz per day.
Jen: Pump the full 20 minutes. I always get a late let down of another ounce or so if I wait it out. Also, a hands-free bra is a lifesaver!
Jennifer: A picture of my baby always helped when I was away from him. Focus on him and how much you love him.
Ann: Relax for sure! Lots of deep breathing and looking at photos of my sweet girl’s chubby cheeks.
Sarah: Staying hydrated (lots of water and coconut water) and pumping at the same times each day.
Stacy: Hands-on pumping (massage and compression), staying hydrated, and changing the cycle speed and angle of the flanges.
Veronica: Watching videos of my little one always made a big impact.
Lydia: Warm compresses, relaxed and comfortable, use the correct flange size and check the suction.
Pumpin' PalsAngelica: Pumpin Pals! Made pumping so much more comfortable!
Ria: Massaging my breasts while pumping almost doubled the amount I could get!
Carmen: Hands on pumping! See the Stanford pumping video about maximizing pumping.
Don't miss our Boob Group podcast episode about Maximizing Your Pumping Sessions!
Common Concerns While Breastfeeding: Why are my nipples white?
Are you feeling a burning sensation in your nipples that creeps up into your breasts? Does this happen most often IN BETWEEN feedings, rather than during your breastfeeding session? Have you noticed that your nipples turn white as soon as your baby pulls off?
What you might be dealing with are vasospasms!
Raynaud’s syndrome, or a vasospasm, is a common phenomenon that affects up to 20% of women of childbearing age. It was originally described as affecting the body’s extremities (hands and feet), but now has been described as affecting many other vessels, including the nipples. The symptoms are often confused with thrush, as both cause a burning sensation in the nipples, yet they are completely different from one another.
Thrush is a yeast infection that can be treated with antifungal treatments (see your article Common Concerns While Breastfeeding: Yikes! Why are my nipples burning?). Vasospasms are constrictions of the blood vessels that usually occur as a result of exposure to cold and are not an indication of an infection. Vasospasms will not be resolved with antifungal treatments.
Are you feeling a burning sensation in your nipples that creeps up into your breasts? Does this happen most often IN BETWEEN feedings, rather than during your breastfeeding session? Have you noticed that your nipples turn white as soon as your baby pulls off?
What you might be dealing with are vasospasms!
Raynaud’s syndrome, or a vasospasm, is a common phenomenon that affects up to 20% of women of childbearing age. It was originally described as affecting the body’s extremities (hands and feet), but now has been described as affecting many other vessels, including the nipples. The symptoms are often confused with thrush, as both cause a burning sensation in the nipples, yet they are completely different from one another.
Thrush is a yeast infection that can be treated with antifungal treatments (see your article Common Concerns While Breastfeeding: Yikes! Why are my nipples burning?). Vasospasms are constrictions of the blood vessels that usually occur as a result of exposure to cold and are not an indication of an infection. Vasospasms will not be resolved with antifungal treatments.
What are vasospasms?
Imagine sitting cross-legged and your foot ‘falls asleep.’ Your foot becomes numb as the blood leaves the area. As soon as you start banging your foot on the floor and ‘waking it up,’ the blood flows back into your foot, causing a sensation of pins and needles. This is the same philosophy with nipple vasospasms. Essentially, as soon as your baby’s warm mouth leaves your nipple, the cold air triggers a vasospasm, causing the blood in your nipple to escape and leave the area. This causes blanching, or whiteness of the nipple, since the blood is constricted. Then, as the blood comes back and starts to flow better, the nipple is ‘woken up,’ causing a burning sensation. This can be extremely painful and frustrating, as the throbbing can be felt throughout the entire day and night.
Symptoms for vasospasms:
- Nipples turn white as baby pulls off from feeding (due to the restricted blood flow to the nipples)
- As blood flows back into the nipples, they turn from white to blue, purple, or red, accompanied by throbbing, burning pain.
- Nipples throb in between feedings, especially when mom feels cold or if she feels a let-down, rather than during a feeding.
It is important to rule out the following, as they can also cause vasospasm-like symptoms:
- Poor latch that compresses and/or pinches the nipple
- Tongue-tie
- Sensitivity to nipple creams
- Thrush/breast infections
- Pregnancy
*** None of these can be treated with vasospasm remedies
Once you have ruled out other causes of vasospasms, you can begin to treat them.
How to treat vasospasms:
- Avoid vaso-constricting substances, such as nicotine, caffeine, and alcohol
- Try to keep your nipples and breasts warm in between feedings. Wool breast pads, such as the ones made by LanaCare, can be fantastic
- Try herbal and vitamin supplements to help increase blood flow and reduce symptoms. My favorite daily regiment is 5000IUs of vitamin D3, 200mg of vitamin B6, the minimum dosage of Natural Calm Magnesium, and Nordic Naturals Omega 3 vitamins.
- Acupuncture – since vasospasms are caused by lack of blood flow to the nipples, acupuncture can help move your blood and keep it from being stagnant in your body
- If none of these measures help with the pain, speak with your doctor about nifedipine, a calcium channel blocker that has vasodilatory effects. Nifedipine, as any medication, has risks of side-effects. These side effects include dizziness, headache, and tachycardia, so please consult your primary healthcare provider.
As always, it can be very helpful to meet with an IBCLC to determine whether your nipple pain is due to vasospasms or to another breastfeeding issue. You can find an IBCLC in your area on the International Lactation Consultant Association website.
Managing Speed-bumps Along Your Breastfeeding Path
This past Saturday, I had the honor of hosting the Breastfeeding Lounge and speaking at the Your Natural Baby Fair about my favorite topic... breastfeeding, of course! The topic for this presentation was a little different than those discussed at the prenatal classes I teach each month. Instead, I was finally able to address all of the questions I am asked at my weekly support group. You know... those questions about hiccups that happen AFTER the initial latch/positioning/initiating milk supply issues. The questions that pop up AFTER the first few months of breastfeeding, right when you think you have it ALL figured out! Now those are truly my favorite!
My presentation was titled: Managing Speed-bumps Along Your Breastfeeding Path. During this talk I focused on:
Appropriate feeding amounts for babies (for up to a year)
Appropriate weight gain for babies (for up to 1 year)
Lactogenic foods that support your milk supply
How to maintain your supply during baby's distractable times, returning to work, and when offering solids
Benefits (both nutritional and emotional) for breastfeeding beyond 1 year
Since this talk could only accommodate 60 people (who happened to be in San Diego at the fair), Sunny, from New Mommy Media and the Preggie Pals podcast, interviewed me to discuss the topics in my presentation.